Chapter 4 – Pain Assessment
Unidimensional Pain Assessment Tools
Unidimensional pain tools assess one element of pain, typically intensity, which refers to the magnitude or the severity of pain. These unidimensional tools are important because they can be used to:
- Provide a baseline of the severity of a client’s pain.
- Determine the need for pain management/treatment.
- Evaluate treatment effectiveness.
For example, if a client has pain, you might manage the pain through repositioning or medication, and then reassess the pain again. Unidimensional pain tools are effective at evaluating pain over time between one time period to the next. However, it is important to note that because they have only one focus, they neglect other dimensions of the pain experience (Lapkin et al., 2021). Another issue is that tools should be selected for each client based on cognitive and cultural factors.
The next sections explore four unidimensional pain tools involving self-report, and that focus on assessing pain intensity.
Numeric Rating Scale
The Numeric Rating Scale (NRS) is a widely used 11-point pain scale from zero to ten (Slomp, 2019). When using the NRS, you commonly ask clients: “On a scale of zero to ten with zero being no pain and ten being the worst pain imaginable, how do you rate your pain?”
The NRS tool is used because:
- It is simple to use.
- It gives a quick assessment of the client’s pain intensity and provides a baseline.
- It is useful for frequent or repeat pain assessments such as after a treatment or medication is provided.
It is the most commonly used pain tool to evaluate pain intensity. However, it is not appropriate to use with young children. The general consensus has been that it can be used with children as young as eight and possibly younger (von Baeyer, 2009). A more recent systematic review found a strong recommendation for its use with children as young as six when assessing acute pain (Birnie et al., 2019). Use of this tool for any client should be based on their developmental age and capacity to engage with numbers. Again, keep in mind that the NRS is unidimensional: it only measures pain intensity at a specific time period (Slomp, 2019).
Visual Analogue Scale
The Visual Analogue Scale (VAS) provides a horizontal (or vertical line) with two anchors. The left side (or bottom) is marked “no pain” and the right side (or top) is marked “worst imaginable pain.” Clients may use their finger to point where on the line where their pain is; digital versions are also now available (see Figure 3).
The VAS is used for similar reasons as the NRS, but it is useful when clients do not resonate with rating pain according to numbers. It is best used with adults considering that a recent systematic review found a weak recommendation for its use with children when assessing acute or chronic pain (Bernie et al., 2019).
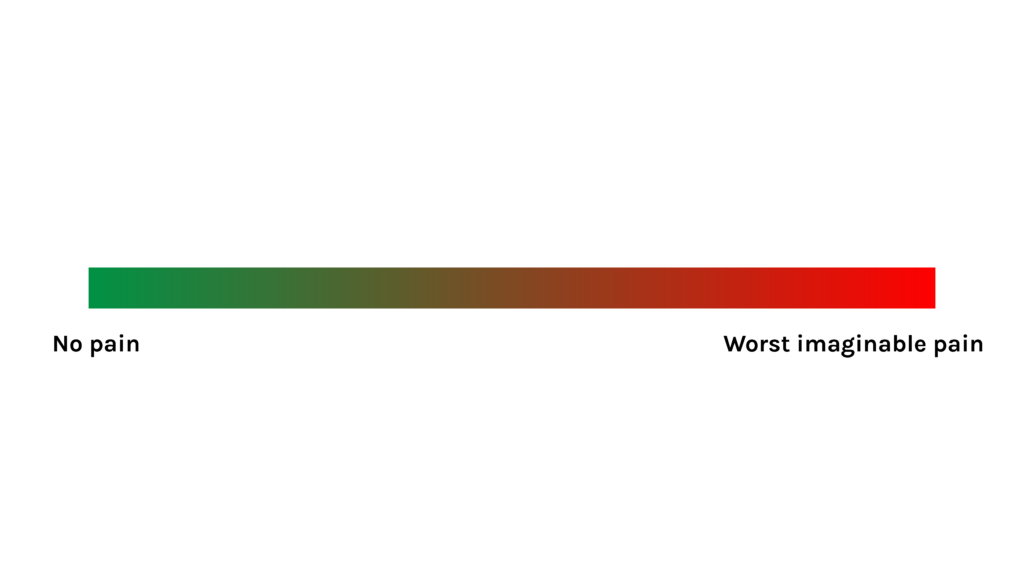
Figure 3: Example of VAS
Verbal Descriptor Tool
The Verbal Descriptor Tool (VDT) provides an opportunity for clients to describe the intensity of their pain using words (Pathak et al., 2018). The client is asked: “Which word best describes your pain intensity?” (Karcioglu et al., 2018). Various versions of the VDT have been developed (see Figure 4): the descriptors often have numbers associated with them, and additional modifiers of the descriptors such as “very mild” and “very severe” can be added.
The VDT is also used for similar reasons as the NRS, but as with the VAS it is useful when a client does not resonate with rating pain according to numbers and prefers descriptors.
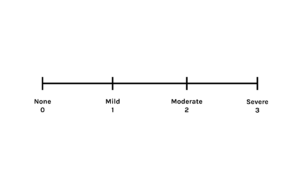
Figure 4: Verbal Descriptor Tool
FACES Pain Scales
Several pain scales involving faces have been developed specifically for children to rate the intensity of their pain. Young children do not have the same cognitive and linguistic capacity as adults, so these types of scales are more developmentally appropriate, particularly for those aged 3–7 years and even older depending on their developmental age. The two most common are the Wong-Baker FACES Pain Rating Scale and the FACES Pain Scale – Revised Version (FPS-R).
The Wong-Baker FACES Pain Rating Scale (Figure 5) is a self-assessment tool that must be understood by the patient, so they are able to choose the face that best illustrates the physical pain they are experiencing. The tool is not for use with infants or patients who are unresponsive. It is not a tool to be used by a third person (i.e., parents, healthcare professionals, or caregivers) to assess the patient’s pain. This tool has actually been used across the lifespan as well including in adolescents and adults.
Ask the child to choose the face that best shows the physical pain they are experiencing. You may need to explain what the faces mean: Face 0 doesn’t hurt at all, Face 2 hurts just a little bit, Face 4 hurts a little bit more, Face 6 hurts even more, Face 8 hurts a whole lot, and Face 10 hurts as much as you can imagine.
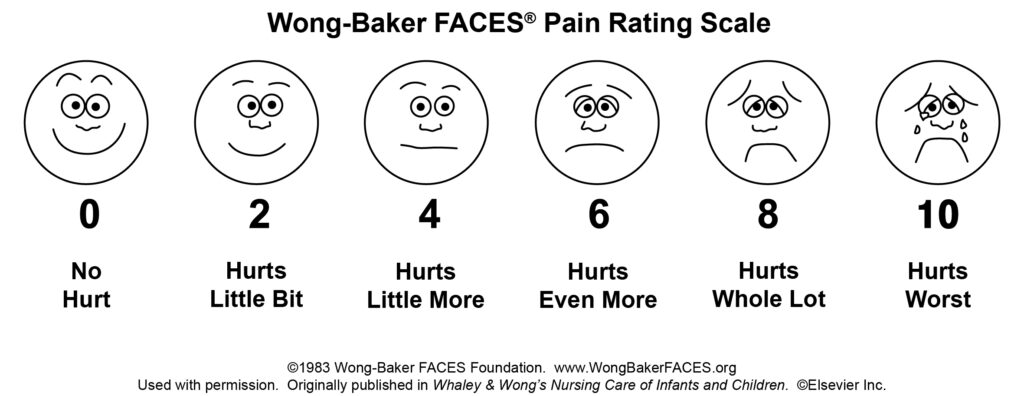
Figure 5: Wong-Baker FACES® Pain Rating Scale Wong-Baker FACES Foundation (2019).
Similarly, the Faces Pain Scale – Revised Version (FPS-R) provides a series of six faces with different expressions to illustrate pain (Hicks et al., 2001) – check out the FPS-R by clicking on the link. This revised version does not include faces with smiles or tears, which can help remove bias; for example, a smiling face may be interpreted as happiness, which does not necessarily mean the individual is not in pain.
When using this scale, say to the child something like: “These faces show how much something can hurt. This face [point to left-most face] shows no pain. The faces show more and more pain [point to each from left to right] up to this one [point to right-most face] – it shows very much pain. Point to the face that shows how much you hurt” you feel right now (Hicks et al., 2001, p. 176).
Based on the findings of a systematic review, the FPS-R is recommended for children as young as seven for acute pain (Birnie et al., 2019).
Contextualizing Inclusivity
Like all tools, including pain tools, the FACES pain scale may not translate to all cultures. The Northern Pain Scale is another adapted version of the FACES scale. It was translated into Inuktitut and recreated with facial expressions and dress to reflect the culture of Inuk people in Canada (Ellis et al., 2011). As a nurse, it is important to consider the use of culturally relevant pain tools.
Sun-Cloud-Pain Scale
Another scale that may be more relevant to assess pain and other symptoms in clients from certain cultures is the Sun-Cloud-Pain Scale. On this scale, 0 indicates that the client feels very well, whereas 5 indicates that the client is feeling very unwell specific to their pain (see Figure 6) (Lapum et al., 2019).
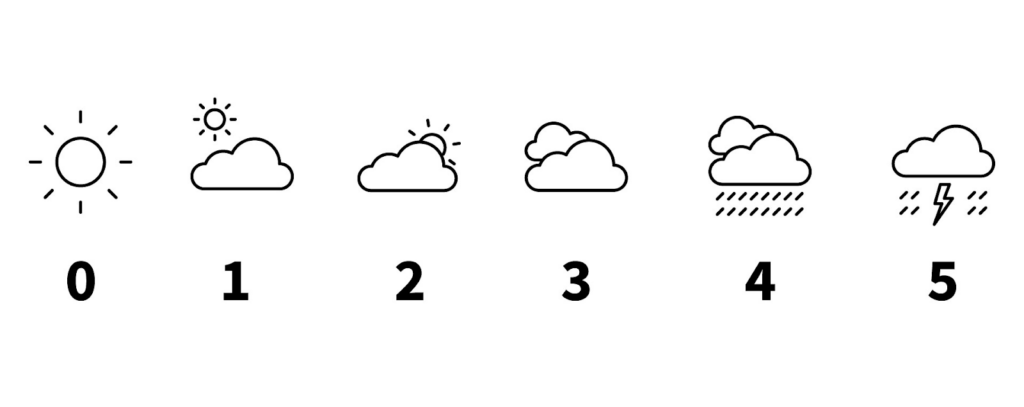 Figure 6: Sun-Cloud-Pain Scale. Graphic created using icons by Linseed Studio from the Noun Project.
Figure 6: Sun-Cloud-Pain Scale. Graphic created using icons by Linseed Studio from the Noun Project.
Activity: Check Your Understanding
References
Birnie, K., Hundert, A., Lalloo, C., Nguyen, C., & Stinson, J. (2019). Recommendations for selection of self-report pain intensity measures in children and adolescents: A systematic review and quality assessment of measurement properties. Pain: The Journal of the International Association for the Study of Pain, 160(1), 5-18. https://doi.org/10.1097/j.pain.0000000000001377
Ellis, J., Ootoova, A., Blouin, R., Rowley, B., Taylor, M., DeCourtney, C., Joyce, M., Greenley, W., Gaboury, I. (2011). Establishing the psychometric properties and preferences for the Northern Pain Scale. International Journal of Circumpolar Health, 70(3), 274-285. https://doi.org/10.3402/ijch.v70i3.17823
Karcioglu, O., Topacoglu, H., Dikme, O., & Dikme, O. (2018). A systematic review of the pain scales in adults: Which to use? The American Journal of Emergency Medicine, 36(4), 707-714. https://doi.org/10.1016/j.ajem.2018.01.008
Lapkin, S. , Ellwood, L. , Diwan, A. & Fernandez, R. (2021). Reliability, validity, and responsiveness of multidimensional pain assessment tools used in postoperative adult patients: A systematic review of measurement properties. JBI Evidence Synthesis, 19 (2), 284-307. https://doi.org/10.11124/JBISRIR-D-19-00407
Lapum, J., St-Amant, O., Hughes, M., Petrie, P., Morrell, S., & Mistry, S. (2019). The complete subjective health assessment. https://ecampusontario.pressbooks.pub/healthassessment/
Pathak, A., Sharma, S., & Jensen, M. (2018). The utility and validity of pain intensity rating scales for use in developing countries. Pain Reports, 3(5), 1-8. https://doi.org/10.1097/PR9.0000000000000672
Slomp, F. (2019). Transforming acute pain experience into a pain score: The challenges. Doctoral dissertation, University of Alberta. https://era.library.ualberta.ca/items/39d68f48-556c-437d-92fb-164063b7a1e3/view/4c3abaf4-92bc-4b1d-83b2-bd14ef7e7fa8/Slomp_Florence_J_201901_PhD.pdf
von Baeyer, C. (2009). Numerical rating scale for self-report of pain intensity in children and adolescents: Recent progress and further questions. European Journal of Pain, 13(10), 1005-1007. https://doi.org/10.1016/j.ejpain.2009.08.006

