Chapter 17 – Ophthalmic System Assessment – The Eyes
Subjective Assessment
Subjective assessment of the ophthalmic system involves asking questions about the health of the client as related to the eye. A full exploration of these pathologies is beyond the scope of this chapter, but common conditions associated with the ophthalmic system include eye trauma (injury to the eye), , , , , , , , , and .
Common symptoms that may be related to the ophthalmic system include vision impairments, eye pain or strain, discolouration, pruritus, swelling, lesions, discharge, dry eyes, and . See Table 1 for guidance on subjective health assessment: many of the questions in the table align with the PQRSTU mnemonic (or variations of it). Try to ask questions in order of importance – you will not necessarily follow the sequential order of PQRSTU.
It is best to begin the assessment by inquiring if the client wears corrective lenses (glasses or contact lenses). If so, ask probing questions such as:
- When did you begin wearing them? Tell me about the reasons you wear them? Do you wear them constantly or at particular times of the day?
- Have you had any issues with them?
- When was your last appointment with an eye specialist?
- Have you had changes in your vision since your last appointment?
Ask the client if they have had eye surgery or any eye trauma such as a physical injury or chemical exposure. If so, assess details surrounding the surgery and/or trauma, how the eye was affected, when it occurred, how it was treated, and whether it continues to affect them.
Always ask about any medications (prescribed or over-the-counter) or supplements the client is taking: name, dose, frequency, reason it was prescribed, and how long they have been taking it.
Remember to ask questions related to health promotion. Depending on the context of the assessment, you may ask these questions and engage in a discussion during a subjective assessment or after an objective assessment. A section on “Health Promotion Considerations and Interventions” is included later in this chapter after the discussion of objective assessment.
Contextualizing Inclusivity – Blindness
Blindness includes a spectrum of visual impairments from partial (low vision) to total blindness. In Canada, legal blindness is defined as “visual acuity of 20/200 or less in both eyes after correction, and/or a visual field of 20 degrees or narrower” (Canadian National Institute for the Blind, 2024).
In the province of Ontario, Canada, the Accessibility for Ontarians with Disabilities Act (AODA) (2005) provides legislation regarding accessibility for people with disabilities, including those who are blind. It includes the requirement that building and healthcare is accessible to people who are blind and accommodations are provided as needed.
As a nurse, you must not make assumptions about the needs and accommodations of a person with visual impairment. Use a cultural humility approach: inquire about how to best support the client and provide accommodations as necessary. For example, health-related material may need to be provided in larger font, in an alternate format such as auditory, or in Braille. As shown in Figure 5, Braille is a tactile system used to read and write, in which patterns of tiny bumps on a page represent letters and symbols (Braille Literacy Canada, 2024).

Figure 5: Braille (Author: Stefan Malmesjö, This file is licensed under the Creative Commons Attribution 2.0 Generic license. Link: https://flickr.com/photos/39061023@N08/4959534304).
Contextualizing Inclusivity: Optometric Screening Examinations
Ask the client when their last eye exam was. They may need frequent optometric screening examinations to support eye health and detect eye conditions. See Table 2 for the recommendations made by the Canadian Association of Optometrists related to eye examinations for clients who are low risk and asymptomatic. Frequencies are increased for individuals who are at higher risk, such as clients with diabetes, macular degeneration, and glaucoma.
These recommendations may be problematic because jurisdictional (provincial and territorial) coverage for eye exams varies in Canada, and do not necessarily include coverage for corrective lenses. For example, OHIP (Ontario Health Insurance Plan) only covers certain age groups and people with certain eye conditions, as discussed in more detail later in this chapter: see section on “optometry (eye-health services)”. Complicating the matter are structural inequities: for example, rural, remote, and Indigenous communities may lack access to eye specialists. As a nurse, you should be aware of any policy changes; for example, OHIP coverage may change. Some clients may have private insurance coverage. You may need to support clients by helping them find additional resources to support eye assessment and corrective lenses.
Table 2: Canadian Association of Optometrists screening recommendations for low-risk and asymptomatic clients.
| Birth to 2 years. | First exam between 6 to 9 months of age. |
| 2 to 5 years. | At least one exam. |
| 6 to 19 years. | Annually. |
| 20 to 39 years. | Every 2 to 3 years. |
| 40 years to 64 years. | Every 2 years. |
| 65 years and older. | Annually. |
Table 1: Common symptoms, questions, and clinical tips.
|
Symptoms |
Questions |
Clinical Tips |
|
Visual impairments is an umbrella term for vision difficulty. Refractive errors are a common type of impairment in which the eye’s shape results in light being incorrectly focused on the retina. These conditions most often include:
Other common eye conditions include:
In addition to blurry vision, other symptoms include:
|
Do you currently have or have you recently had any difficulty seeing? You may need to ask specific questions about the presence of: blurry vision, double vision, floaters like black dots that move across their eyes, blind spots, colourful circles such as a rainbow around light sources like a streetlight, and difficulty seeing at night or in a dimly lit environment. If the responses are affirmative, you might need to provide additional probes: Quality/quantity: Can you describe it? How bad is it? Timing/treatment: When did it begin? Did it begin suddenly or gradually? Is it constant or intermittent? If intermittent, how long does it last? Have you seen a doctor for it? Has it been treated? Provocative/palliative: What makes it better? What makes it worse? Understanding: Do you know what is causing it? |
All people have occasional floaters; these become more frequent with age. To assess the seriousness, ask whether there has been a sudden increase in the number of floaters and whether they are permanent and/or associated with flashes of light or a dark shadow like a curtain. Refer clients experiencing halos to a physician because halos can be associated with specific eye diseases. Prompt attention may be needed if halos are associated with other symptoms such as pain and blurred vision. Diplopia may also be indicative of an urgent condition such as a cerebral bleed (stroke, aneurysm) so immediate referral is required, particularly when associated with related symptoms such as confusion, slurred speech, weakness, and dizziness. As the nurse, you should immediately notify the physician or nurse practitioner and conduct a primary survey |
|
Eye pain or eye strain are unpleasant sensations. Eye pain is subjectively described in many ways such as tenderness, discomfort, burning, throbbing, stabbing, and sharp pain on, around, or behind the eye. Pain can be associated with trauma, infection, corneal abrasion, foreign body, and glaucoma. Eye strain is described as tired and achy eyes. It can sometimes be associated with looking at something for a long period of time such as a computer screen or wearing an incorrect or new corrective lens prescription. |
Have you recently had any eye pain or eye strain? If yes, do you currently have it now? If the responses are affirmative, you might need to provide additional probes: Region/radiation: Where is it located? Is it in one or both eyes? Does it radiate anywhere? Quality/quantity: What does it feel like? How bad is it? Severity: Can you rate it on a scale of 0 to 10 with 0 being no eye pain (or strain) and 10 being the worst you have ever had? Provocative/palliative: Is there anything that makes it worse? Is there anything that makes it better? Timing/treatment: When did it begin? Did it begin suddenly? What were you doing when it began? Is it constant or intermittent? How often do you get it? Have you taken anything to treat it? Have you taken any medications? Understanding: Do you know what is causing it? Other: How does it affect your daily life? |
Eye pain can have many causes. The cause may be obvious as the client may have experienced an injury. Refer clients to a physician or nurse practitioner if they have had recent eye surgery or a history of glaucoma or the pain is:
Eye strain is a common symptom today because of the increased use of computers and smartphones. One common recommendation is that individuals should limit screen time and follow the 20-20-20 rule: every 20 minutes, take a 20-second break to focus on something approximately 20 feet away to help relax the eye muscles. |
|
Discolouration (erythema, jaundice), pruritus, swelling, and lesions (open sores, bumps). Discolouration is often associated with the sclera of the eye or lesions surrounding the eye. For example, a client might tell you that the whites of their eyes are reddened or have become yellow. Pruritus may be generalized over the area of the whole eye or associated with a specific lesion on the eyelid. Lesions can be small bumps that are often red with evidence of swelling. Lesions can also be open sores that may be draining discharge. |
Have you noticed any discolouration of your eyes or around the eyes (such as redness or yellowish colour)? Have you noticed any swelling (or itching, sores, or bumps) on or around the eye? If the responses are affirmative, you might need to provide additional probes: Quality/quantity: Tell me about it? What does it look like? What does it feel like? How bad is it? Region/radiation: Where is it located? Has it extended into other areas? Severity: Pruritus is the only one of these symptoms you might ask a client to rate on a scale of 0 to 10. Provocative/palliative: Is there anything that makes it worse? Is there anything that makes it better? Timing/treatment: When did it begin? What were you doing when it began? Is it constant or intermittent? How often do you get it? Have you taken anything to treat it? Have you applied anything on the eye to treat it? Have you taken any medications? Understanding: Do you know what is causing it? Other: How does it affect your daily life? When asking about open sores, you may ask about any discharge and the colour. |
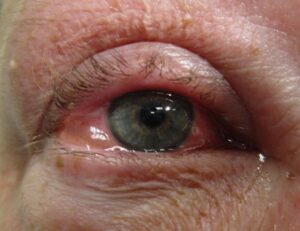
Conjunctivitis (pink eye) is a condition in which the sclera become red. Erythema can appear around the eye. With darker skin tones, erythema may appear reddish/purple in colour. With very dark skin tones, it may be difficult to visualize. With lighter skin tones, erythema is typically dark pink to red. Conjunctivitis can be caused by allergies or contact with chemicals (make-up, chlorine) and be accompanied by related symptoms such as pruritus and swollen eyes. It can involve bacterial or viral infections. When the cause isn’t obvious (like allergies), refer the client to a doctor or nurse practitioner. Tell clients to wash their hands well, avoid touching their eyes, and avoid sharing anything that touches their eyes such as towels and make-up. If relevant, advise clients to remove their contact lenses.
By Microrao – Own work,
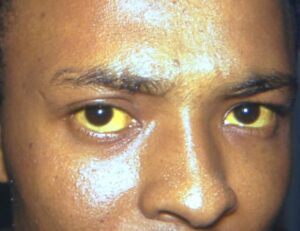
By James Heilman. This file is licensed under the Jaundice can result in the yellowing of the complete sclera. It can cause pruritus and skin discolouration. In persons with darker skin tones, the discolouration may be subtle or go unnoticed but visible in the sclera as shown in image below. In persons with lighter skin tones, jaundice can appear yellow or even orange in colour. Jaundice can be associated with infections, cancer, and other conditions affecting the liver, pancreas, and gallbladder. Always report this finding to the physician or nurse practitioner as it can be a sign of a new disease or the advancement of a disease.
Taken from https://phil.cdc. Blepharitis is an inflammatory condition in which the eyelids appear red and sometimes swollen and irritated. It is usually caused by an excessive amount of bacteria or clogged oil glands on the eyelids.
This work has been released into the public domain by its author, clubtable, at the German |
|
Discharge, dry, or gritty eyes are symptoms that can be associated with a variety of conditions. Small amounts of clear eye discharge can be normal: clients might wake up with a small amount of crusted mucous on the side of the eyes. However, persistent watery eyes can be associated with allergies, blocked lacrimal apparatus (tear duct), and infections. Yellow, green, or white discharge can be associated with infections and appear as mucous or crusty debris around the eyes, often associated with erythema and swelling. Dry eyes can occur when the lacrimal gland doesn’t make sufficient tears to irrigate the eyes. It can be associated with a burning, gritty, scratchy feeling. Dry and gritty eyes are commonly associated with aging and hormonal changes, but can also be associated with certain medications, environmental conditions, or diseases that affect normal blinking |
Have you noticed any discharge from your eyes? Have you had any problems with dry or gritty eyes? If the responses are affirmative, you might need to provide additional probes: Quality/quantity: Tell me about it? What does it feel like? How bad is it? Region: Where is it located? Provocative/palliative: Is there anything that makes it worse? Is there anything that makes it better? Timing/treatment: When did it begin? What were you doing when it began? Is it constant or intermittent? How often do you get it? Have you taken anything to treat it? Have you taken any medications? Understanding: Do you know what is causing it? Other: How does it affect your daily life? |
Refer any client with eye discharge, particularly when not associated with allergies, to a physician or nurse practitioner.
This file is licensed under the |
|
Other symptoms can include headache, fever, light sensitivity (photophobia), twitching, confusion, and nausea and vomiting. |
Have you experienced any headaches? Ask about other symptoms: use variations of the PQRSTU mnemonic to assess symptoms further if the client’s response is affirmative. |
These symptoms can be related to other body systems and non-ophthalmic issues. Conduct a focused assessment on the related body systems. |
|
Personal and family history of conditions such as refractive errors, cataracts, glaucoma, diabetic retinopathy, and retinal detachment. Always inquire whether the client has had any eye injuries. |
Do you have any chronic eye conditions? Do you have a family history of any of these conditions? If the responses are affirmative, you might need to provide additional probes: Tell me about the condition. When did the symptoms begin? When were you diagnosed? How has it been treated? How well did the treatment work? How are you managing it? |
The biological and non-biological nature of family may be important to explicate when asking questions, considering that the risk factors may be influenced by genetics and/or culture. This assessment will help you gain a better understanding of the client and determine appropriate interventions and education.
|
Priorities of Care
Any eye trauma or sudden change in vision is a priority of care. Changes may include blurry vision, dark spots, shadows or a dark curtain across the central or peripheral vision, dim, distorted or double vision, or halos or flashing lights. These may require immediate treatment to avoid permanent damage to vision, among other consequences. For example, sudden changes to vision may be related to a stroke, retinal tears, detachments, or hemorrhages. Conduct a primary survey and report the findings to the physician or nurse practitioner. Prompt attention is also needed when clients report eye pain, conjunctivitis, and any symptoms suggestive of infections such as purulent discharge, redness, and swelling.
Cultural Inclusivity
In some cultures, certain substances are used for newborn eye care in the first 24 hours following birth (Osman et al., 2018). Approach this kind of tradition with cultural humility, but also ensure patient safety with regard to how these substances may affect the integrity of the eyes and vision. Additionally, some individuals use over-the-counter eye drops when they have dry, red, and/or itchy eyes. Some of these eye drops can constrict the vasculature, not address the actual problem, and actually worsen the issue (Mukamal, 2024). Consider referring the client to the physician or nurse practitioner to discuss their symptoms and find safer alternatives. If the client has used eye drops for more than a few weeks or the client is uncertain of the cause, refer them to an eye doctor for a proper diagnosis and effective treatment.
Activity: Check Your Understanding
a condition when the sclera and the area around the eye becomes red, sometimes it is infectious.
are a condition in which the eye has problems bending and focusing light appropriately onto the retina (back of the eye) making it difficult to see.
are when the eye's lens becomes cloudy resulting in symptoms such as blurred vision. Often caused by the breakdown of proteins in the eye that happens at the age of 40 to 60 and older.
is the build-up of fluid and intraocular pressure that damages the optic nerve resulting in blindness.
refers to damage to the macula in the back of the eye (retina) that results in the loss of central vision.
is an emergency situation when the retinal tissue pulls away from the back of the eye (without immediate treatment it can result in permanent loss of vision).
is when the vitreous pulls away from the retina resulting in floaters and flashes of light (the vitreous is a jelly-like substance that fills the inside of the eye and is connected to the retina). Although in of itself is not serious, it can cause retinal detachment.
a disease caused by diabetes in which high blood sugar levels damage the retina's blood vessel resulting in vision impairment such as dark spots floating across the eyes, blurred vision, and vision loss.
is the reduced ability to see colour or distinguish between colours, sometimes referred to as colour blindness.
refers to the sensation that there is some sort of grit or sand in the eyes.
is nearsightedness meaning that distant objects are blurry.
is farsightedness meaning that close-up objects are blurry
is an irregular-shaped cornea/lens that results in close-up and distant objects being seeing as out-of-focus (not as sharp) and appearing blurry.
refers to a condition that affects the aging eye (40 to 50 years of age) resulting in difficulty seeing close-up objects (objects become blurry).
is misalignment of the eyes in which they don't work together because one is pointed in a different direction. This results in double vision, poor revision, and amblyopia (image suppression from the affected eye meaning that the brain relies on the unaffected eye's vision). Often clients are born with it or develop it at a young age, but adults can also develop it as a result of neurological conditions.
is sometimes referred to as lazy eye and involves image suppression from the affected eye meaning that the brain relies on the unaffected eye's vision. One main cause is strabismus.
are small dots or wiggly lines that move across a person's vision. They are composed of cellular debris within the eye's vitreous.
are colourful circles (like a rainbow) around light sources such as a streetlight.
is double vision in which two of the same image are seen.