Chapter 17 – Ophthalmic System Assessment – The Eyes
External Eye Assessment and Anterior Eyeball Assessment
The external eye assessment and anterior eyeball assessment includes assessing all visible eye-related structures: the area surrounding the eye, the eyelids, and the anterior eyeball. The assessment includes:
-
- General Inspection
- Pupillary light reflex and accommodation.
General inspection
This assessment should be done with the client looking straight ahead. Steps in the assessment include:
- Inspect for symmetry and placement of the eyebrows, eyes, eyelids, and .
-
- Normally, the eye area is symmetrical, with the eyebrows and eyes at the same level on the left and right side. The upper eyelids should cross the and sit above the pupil so that you can see some of the upper iris (i.e., iris above the pupil). The palpebral fissures should be equal bilaterally, and you should observe even distribution of eyelashes and eyebrow hair. Symmetry is a normal finding, but be aware that eye shape varies by ethnic background and can include eyes that are upward- or downward-turned, round, or almond-shaped, with a monolid or double eyelid.
- Describe the appearance and location of any asymmetry such as eyelid drooping or retraction or unequal palpebral fissures. Describe any loss of eyelashes or loss of hair across eyebrows.
- Inspect eyeball alignment in sockets.
-
- Normally, eyeballs are aligned in the eye socket and are not protruding or sunken. See Figure 6.

Figure 6: Aligned eyeballs. (Photo by ABSOLUT on Unsplash: weblink).
-
- Abnormal findings may include protrusion of the eyeballs in which they bulge out of the socket (medical term: exophthalmos, also known as proptosis). This can be associated with eyelid retraction in which you can see visible sclera above the iris. The most common cause of this is . Another abnormal finding is sunken eyeballs (medical term: enophthalmos). This can be associated with age in which the client experiences atrophy around the eye, but it can also be associated with other conditions such as physical trauma.
Video 1: Inspection for symmetry and placement of the eyebrows, eyes, eyelids, and palpebral fissures and inspection of eyeball alignment [0.43 seconds].
- Inspect for , swelling, and discolouration (such as redness) of the eyelids and around the eyes.
-
- Normally, you will not observe lesions, swelling, or discolouration, but be aware that some lesions are normal. For example, freckles and nevi can be considered normal, but you should always use the ABCDE mnemonic to assess. are caused by sun exposure and may appear on the face around the eyes. The area around the eyes is normally the same colour as the rest of the face, although the skin below the eyes may be a slightly darker shade.
- If present, describe the appearance and location of any lesions, swelling, and discolouration. Common lesions associated with swelling and redness include and . Intraocular hemorrhage (bleeding in the eye) can be visualized in the sclera of the eye and caused by conditions such as physical injury or retinal detachment.
- Inspect for any discharge associated with the eyes.
-
- Normally, you will observe no discharge, although a small amount of crust around the eyes (sometimes called “sleep”) is normal after first waking up.
- If present, describe the colour (clear, purulent, sanguineous, serosanguineous), consistency (thin, thick, stringy), quantity (mild, moderate, severe), and location of discharge.
Video 2: Inspect for lesions, swelling, discolouration and discharge. [0.27 seconds].
- Inspect the cornea, lens, and sclera on the anterior eyeball. It can be helpful to look directly at the eyeball from the front of the client and also look at the eyeball when standing at the side of the client while shining a penlight tangentially across the eyeball in order to better visualize the eyeball.
-
- Normally, the cornea are smooth and the lens and cornea are clear. The sclera may be white or may have a soft (muted) greyish-blue tone in clients with darker skin (see Figure 7). You may observe flat small brown specs (freckles) on some sclera (Figure 8), particularly in clients with darker skin tones.
- Abnormal findings include corneal abrasions (scratches), which are often painful. The cornea and lens may be cloudy, sometimes having a milky appearance (Figure 9).


Figure 7: Greyish-blue tone (left) and white tone (right) sclera.
Image on left: Author: By Basile Morin – Own work, CC BY-SA 4.0, https://commons.wikimedia.org/w/index.php?curid=105228490
Image on right: Author: 8thstar at English Wikipedia, Creative Commons Attribution-Share Alike 3.0 Unported license, https://commons.wikimedia.org/w/index.php?curid=1944750)

Figure 8: Freckle on sclera.
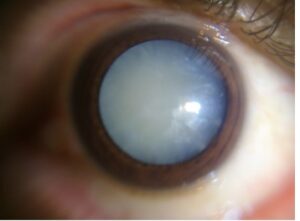
Figure 9: Cloudy lens (probable diagnosis: cataract).
(Author: Imrankabirhossain, Creative Commons Attribution-Share Alike 4.0 International license, from: https://commons.wikimedia.org/wiki/File:Intumescent_cataract.jpg).
- Inspect the conjunctiva of the inside of lower and upper eyelids. Place the pads of your thumbs below the client’s eyelids (on the orbital bone) and gently pull downward. Ask the client to look up towards the ceiling while inspecting the inner lower eyelid. Next, place the pads of your thumbs on the orbital bone above the eye and gently pull upward. Begin by inspecting the inner upper eyelid, and then ask the client to look to the right and then to the left while you inspect the outer and inner canthus.
-
- Normally, the conjunctiva is transparent with a slightly pink colour particularly over the area that covers the inside of the lower eyelids, visible blood vessels, and no lesions, swelling, or foreign bodies (Figure 10).
- Describe the location and appearance of any lesions, swelling, foreign bodies, or discolouration. See Figure 11 for an example of a melanoma.

Figure 10: Transparent conjunctiva with a slightly pink colour, visible blood vessels, no swelling or foreign bodies, small brown macule on right eye medial to the limbus, no other lesions.
(By http://commons.wikimedia.org/wiki/User:Brazilianboy94 – Own work, CC BY-SA 4.0, https://commons.wikimedia.org/w/index.php?curid=80905686)
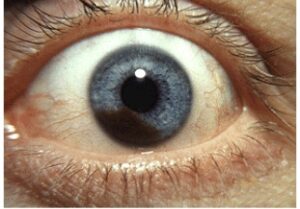
Figure 11: Melanoma.
(Author: Jonathan Trobe, Creative Commons Attribution 3.0 Unported license, from: https://commons.wikimedia.org/wiki/File:Iris_melanoma.jpg).
Video 3: Inspect the Cornea, Lens, Sclera, and Conjunctiva. [1.06].
- Note the findings:
-
- Normal findings might be documented as: “Eyebrows, eyes, eyelids, and palpebral fissures symmetrical. Even distribution of eyebrows and eyelids. Normal alignment of eyeballs with no protrusion or sunken eyeballs. No lesions, swelling, and discolouration of eyelids and around eyes. No eye discharge. Smooth cornea with no abrasions, lens and cornea are clear with white sclera and no lesions. Conjunctiva are transparent with a slightly pink colour, no lesions, swelling, or foreign bodies.”
- An abnormal finding might be documented as: “Drooping left eyelid.”
Contextualizing Inclusivity
Periorbital hyperpigmentation (sometimes referred to as “circles” under the eyes) and puffiness (sometimes referred to as “bags” under the eyes) can be genetic, worsen with age (natural atrophy in which the skin begins to sag), and be influenced by other factors such as lack of sleep, allergies, dehydration, and fluid retention. The skin under the eyes is thin and transparent, so the underlying structures (vasculature) can create darkness under the eyes in which the pigmentation may vary in shades from brown, black, blue, and purple. People with darker skin often have hyperpigmentation around the eyes and darker circles under the eyes related to genetics, while the underlying structures may be more prominent in people with lighter skin.
False Eyelashes were invented more than 100 years ago, but have become a more common cosmetic enhancement in the last 20 years. If a client wears false eyelashes, assess the eyelids for any signs of inflammation, as long-term use without breaks can block the glands and damage the follicles. Remember to use an inclusive assessment approach because false eyelashes are a gendered and racialized beauty trend that can lead to judgement and discrimination.
, when bilateral, is common with age due to muscle atrophy around the eye. It can also occur in children; if a child is born with it, the ptosis is typically congenital. Surgery may be considered, particularly if it affects vision.
Note that eyebrows change with age: hormonal changes beginning in the 40s can lead to thinning eyebrows (particularly the outer third) in women and more bushy eyebrows and stray hairs in men.
Dry eyes can affect people of all ages, but this condition is common in older adults and people experiencing menopause because the lacrimal apparatus production of tears is reduced. This condition can also be caused by adverse effects to medical treatment; it can lead to watery eyes, along with erythema and itchiness.
Some clients may have an ocular prosthesis (an artificial eye, as shown in Figure 12). These are typically made of an acrylic material and customized for a person’s eye socket. The quality of these vary, but many look quite real. In the province of Ontario (Canada), the costs are covered by OHIP (see artificial eyes). Explain to clients that prostheses must be removed and cleaned regularly and will require replacement after developmental changes, especially childhood growth spurts.

Figure 12: Ocular prosthesis.
(By MalastiC, from https://commons.wikimedia.org/wiki/File:Colocaci%C3%B3n_Protesis_Ocular_4.jpg, the Creative Commons Attribution-Share Alike 4.0 International license.).
Priorities of Care
Report any abnormal findings to the physician or nurse practitioner.
In certain cases, findings should be reported immediately:
- New onset of drooping eyelid could be a potential sign of stroke. Conduct a primary survey and a focused neurological and eye assessment.
- If you observe an intraocular hemorrhage, begin with a primary survey, followed by an eye assessment, and sometimes a brief scan of the neurological system.
Loss of eyebrow hair or eyelashes is usually not a major concern. However, if the client is also experiencing thinning hair or hair loss on their scalp, along with other symptoms such as fatigue and weight change, you should investigate further.
Eye hordeolum and chalazions may be treated by applying warm compresses. If they don’t disappear within a few days, you should investigate further.
Pupillary light reflex and accommodation
The pupillary light reflex is used to assess the eye’s response to light and innervation of CN II (optic) and CN III (oculomotor) while testing for accommodation assesses the eye’s ability to accommodate for near objects and innervation of CN III (oculomotor). These assessments usually begin with the pupillary light reflex (Video 4) followed by accommodation (Video 5), as described below:
- To test pupillary light reflex, ask the client to look straight ahead at a distant point on the wall behind you (i.e., at the opposite end of the room) to slightly dilate the pupils. If possible, also reduce the lighting in the room to dilate the pupils.
- First, assess the pupils for shape, equality, and size.
-
- Normally, the pupils should be round, equal in size and shape, and sized 2 to 8 mm in diameter (Figure 13). Normal size will depend on the ambient lighting; for example, the diameters of normal pupils are smaller in a well-lit environment (2–4 mm) and bigger in a darker environment (4–8 mm).
- Abnormal findings may include pupils that are not round, are unequal in size and shape, or are smaller (: Figure 14) or larger (: Figure 15) than the normal size.

Figure 13: Normal pupil size.
(By Biswarup Ganguly, https://commons.wikimedia.org/w/index.php?curid=10066382, Creative Commons Attribution-Share Alike 3.0 Unported license.)

Figure 14: Miosis.
(By Thomas Bonini, from: https://commons.wikimedia.org/wiki/File:Miosis_caused_by_opium_consumption.jpg, Creative Commons CC0 1.0 Universal Public Domain Dedication)

Figure 15: Mydriasis.
(By Nutschig at the English-language Wikipedia, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=137216882)
- Ask the client to continue looking straight ahead at the distant point on the wall. Turn on your penlight and move it from the right side of the client to directly in front of their right eye. Shine the penlight on the eye, pause for 1–2 seconds, and then move the light back out to the side: the light should activate CN II to send a message to the brain, and then CN III should send a message to the pupillary muscles causing pupillary constriction.
When pausing the light on the eye, observe the client’s right eye and left eye for pupillary constriction. If necessary, perform this procedure twice so that you can focus on the right eye (for direct response: meaning the pupil of the eye on the side where the light is introduced constricts), and then focus on the left eye (for consensual response: meaning the pupil of the opposite eye where the light is introduced also constricts). Repeat this step for the left eye and observe direct and consensual responses. Also note the size of the pupil afterwards: it should return to the same size as before the light was introduced.
-
- Normally, you should see a direct response and a consensual response of both eyes. Normal constriction is often described as prompt or brisk, meaning it happens right away. Normally, when you remove the light, pupils will return to the same size/shape they had before you introduced the light.
- Abnormal findings include no direct and/or consensual response (response is absent and pupils do not constrict), or when pupillary constriction is sluggish (slow).
Video 4: Pupillary light reflex test. [0.25 seconds].
- To test accommodation, first ask the client to stare straight ahead at a distant point on the far wall and if possible, have the lights dimmed to dilate the pupils. While they are staring straight ahead, explain that you are going to move your index finger (or your penlight turned off) in front of their nose and slowly bring it closer to their nose. Ask them to shift their gaze from looking at the distant point on the wall to your finger and stay focused on your finger. Next, place your index finger in front of their nose (about 20–30cm from the tip of their nose and slowly move it closer so that it is about 8 cm from the tip of their nose).
-
- Normally, the client should shift their gaze to your finger (convergence of the eyes inward) accompanied by pupillary constriction.
- Abnormal findings include inability to shift eyes simultaneously and lack of pupillary constriction.
Video 5: Testing for accommodation. [0.37 seconds].
- Note the findings:
-
- Normal findings might be documented as: “Pupils round, 3 millimetres, and equal in size. Prompt, direct and consensual light reflex noted bilaterally. When testing for accommodation: pupillary constriction and convergence of eyes noted.” (In some institutions, this is sometimes noted as PERRLA: pupils equal, round, and reactive to light and accommodation.)
- Abnormal findings might be documented as: “No direct or consensual light reflex noted bilaterally.”
Contextualizing Inclusivity
It can be difficult to evaluate the pupil size and pupillary constriction in clients with dark irises. If necessary, ask them to look up while doing the assessment; this can help. Alternatively, use a second penlight and shine the light tangentially to highlight the iris without causing an unintentional pupillary reflex.
Prioritizing Care
One serious finding is a “blown” pupil: the pupil is dilated and also fixed and unresponsive. This condition resembles mydriasis, as shown above in Figure 15; it is often associated with brain herniation, meaning the brain tissue shifts due to increased intracranial pressure. Brain herniation can be related to various pathophysiological processes such as brain trauma, stroke, aneurysm, or tumour. New onset of unilateral or bilateral fixed and dilated pupils should be immediately reported to the physician or nurse practitioner: as the nurse you should stay with the client and complete a primary survey.
Anisocoria (unequal pupil size) Figure 16, image below, does not require treatment unless it is new onset. Many clients have unequal pupil size, but new onset anisocoria may be of concern because it can be associated with neurological problems, stroke, infection, or eye trauma. Complete a focused assessment and report the findings to the physician or nurse practitioner.

Figure 16: By Tair1978 – Own work, Creative Commons Attribution-Share Alike 4.0 International license, from: https://commons.wikimedia.org/w/index.php?curid=82053909).
Activity: Check Your Understanding
are the opening/space between the upper and lower eyelids.
refers to the border between the cornea and the sclera, looks like a darker ring around the iris.
is a disease involving an overactive thyroid gland leading to high levels of thyroid hormone in the blood.
A general term referring to an abnormal appearance or growth.
are flat, irregular shaped macula that are slightly darker than the client's normal skin colour and found on sun-exposed areas of the body.
are small, red, and painful bumps on the eyelid often caused by bacterial infections (commonly called styes).
small red and swollen bumps, sometimes painful, caused by blocked oil glands that clog up.
refers to the drooping of the upper eyelid over the eye.
refers to excessive constriction of pupil.
refers to excessive dilation of the pupil.

