Chapter 17 – Ophthalmic System Assessment – The Eyes
Ophthalmoscope Examination
Use an ophthalmoscope examination (see Figure 24) to assess the presence of any . Assess the ocular fundus (back of the eye) structures such as the retina, the macula, optic disc, and the vasculature (artery and vein; see Figure 25).
One component of the ophthalmoscope exam involves assessing the . This test was originally – and inaccurately – called the “red reflex” based on the colour of light reflected from the back of the eye in white babies. The ophthalmoscope has a light that is directed onto the pupil to highlight this reflex.
Conduct this assessment with the client standing or sitting on the edge of the examination table. Again, position yourself so that your eyes are at the same level as the client’s. If relevant, both you and the client should remove eyeglasses as these can obstruct assessment. The ophthalmoscope has different types of lights: the medium circle is usually sufficient for the purposes of a nursing assessment. Brighter lights are more uncomfortable for clients, so always use the least brightness possible.
Begin by comparing the ocular fundus reflexes in the left and right eyes as follows:
- Ask the client to look straight ahead at a distant point on the wall behind you (i.e., at the opposite end of the room) to slightly dilate the pupils and keep eye structures still. If possible, reduce the lighting in the room to dilate the pupils.
- Hold the ophthalmoscope in your dominant hand.
- Look through the viewing aperture as you place the ophthalmoscope against your orbital and cheek bone on your dominant side.
- You may need to adjust the lens selector dial to focus so the image is clear (if it is your first time, try this out first by focusing on a few objects in the room).
- Stand 15 degrees lateral to the eye that will first be assessed and place your opposite hand on the client’s forehead above their eye, with your arm extended about 30 cm away from the client.
- Direct the light on the client’s pupil and observe the ocular fundus reflex.
- Then repeat on the other eye so that you can compare.
-
- Normally, the ocular fundus reflexes are present in both eyes and are symmetrical in terms of colour and intensity (brightness). Colour varies by pigmentation:
- Clients who have darker skin colour often have darker reflexes that appear as green or blue.
- Clients who have medium skin colour often have reflexes that appear as orange to yellow.
- Clients who have lighter skin colour often have reflexes that appear red to orange. (WE C Hope, 2023).
- Normally, the ocular fundus reflexes are present in both eyes and are symmetrical in terms of colour and intensity (brightness). Colour varies by pigmentation:
-
- Abnormal ocular fundus reflex findings may include asymmetry in terms of colour and intensity, a dark patch, and/or one or both eyes having an absent/black, dull or white reflex. These findings can be associated with eye conditions such as cataracts, infections, tumours, retinal detachment, hemorrhage, and cornea abrasion. Report all abnormal findings to the physician or nurse practitioner.
8. Note the findings:
-
- Normal findings might be documented as: “Ocular fundus reflex present in both eyes and symmetrical in colour and brightness.”
- Abnormal findings might be documented as: “Ocular fundus reflex asymmetrical, left eye shows whitening of reflex.”
The second step in this examination is assessment of the ocular fundus. This assessment is usually done by a physician, but nurses may also complete it. Follow steps 1–6 above and then continue to hold the ophthalmoscope against your orbital and cheek bone while slowly moving in and maintaining focus on the ocular fundus reflex until you can view the ocular fundus. This part of the examination involves assessing the optic disc. Normally, it will be round/oval in shape with demarcated boundaries (no blurring) and yellow-orange-pink in colour (no paleness or dark spots). You should also assess the other areas of the fundus, including the retina, retinal vasculature, and macula.

Figure 24: Ophthalmoscope – viewed on the left.
(By James Heilman, MD – Own work, Public Domain, https://commons.wikimedia.org/w/index.php?curid=4398920)
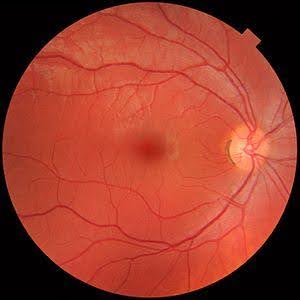
Figure 25: Ocular fundus
(By: Häggström, Mikael (2014). “Medical gallery of Mikael Häggström 2014“. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.008. ISSN 2002-4436. Public Domain. or By Mikael Häggström, used with permission. – Own work)
Contextualizing Inclusivity
The continued use of “red reflex” terminology reflects unconscious bias and a tendency to use the white body as the norm in nursing and medicine. It is important to challenge this racist discourse and use the term “ocular fundus reflex” in order to shift this language and advocate for more inclusive approaches to ophthalmological examinations.
Prioritizing Care
Any abnormal findings related to the ocular fundus reflex or the ocular fundus require specialist examination. Always report abnormal findings to the physician or nurse practitioner.
Activity: Check Your Understanding
References
WE C Hope (2023). Fundal (red eye) reflex and red-eye reduction. https://wechope.org/retinoblastoma/white-eye-reflex/what-causes-red-eye/
refers to the loss of transparency when the cornea becomes opaque (cloudy) due to damage or scarring.
is the reflection of the ophthalmoscope light from the back of the eye.

