Chapter 17 – Ophthalmic System Assessment – The Eyes
Central Visual Acuity Assessment
Central visual acuity refers to the clarity or sharpness of vision in the centre field of view as a client looks straight ahead. Testing for central visual acuity can assess distance vision (far-away objects, e.g., for driving or reading a chalkboard at school) or near vision (close-up objects, e.g., for reading). Put simply, central visual acuity is the ability to see, and is innervated by CN II (the optic nerves).
Distance vision
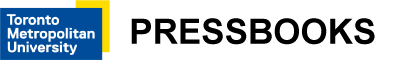
Evaluating visual acuity for distance vision is easily assessed using the Snellen eye chart (see Figure 17). The steps include:
- In a well-lit environment, have the client stand 20 feet away from the Snellen eye chart. The chart should be placed on the wall at eye level, about 5–6 feet from the floor. If the client uses glasses or contact lenses for distance, they should leave them on/in during this test. Snellen eye charts are also available in 10-feet format; in this case, the client stands 10 feet away from the chart.
- Ask the client to fully cover one eye with the palm of their hand or an eye occluder if you have one.
- Ask the client to read as many lines as they can, without squinting, beginning with the top line and reading one line at a time. If necessary, you may point to the line.
- When the client states they have read as far as they can, ask them to try to read the next line.
- If they make an error on a line, ask them to repeat the line. Clients may make a maximum of two errors on a line in order for their visual acuity to be identified on that line; if they make more than two errors, their visual acuity is noted as the line above.
- Note the client’s visual acuity using a fraction: the numerator (top number) is the distance the client is standing from the chart and the denominator (bottom number) is the distance at which a person with normal vision can read that line as noted on the Snellen eye chart (Canadian Association of Optometrists, 2023; Porter, 2022). According to the standard Snellen eye chart, normal vision is 20/20, meaning the client can read at 20 feet what a person with normal/good vision can read at 20 feet (Porter, 2022). Record the denominator as the last line the client could read with a maximum of two errors on the line. Record the eye (left or right), how many letters they missed, and whether or not they were wearing glasses or contact lenses (see Clinical Tip textbox for more information).
- Repeat steps 2–6 for the other eye.
-
- As noted above, normal visual acuity is 20/20 (Porter, 2022).
- Abnormal visual acuity can involve cases in which the denominator is bigger, and sometimes where the numerator is smaller. For example, 20/60 means that the client can read at 20 feet what a person with normal/good vision can read at 60 feet. Sometimes a client cannot read any letters at 20 feet: if so, ask them to move closer to the chart (i.e., 10 feet from the Snellen eye chart) and try again. In this case, the numerator would be recorded as 10. As an example, you may report vision as 10/80, meaning that the client can read at 10 feet what a person with normal/good vision can read at 80 feet.
- Note the findings:
-
- Normal findings might be documented as: “Visual acuity 20/20 -1 in both eyes with contact lenses.” (Here, -1 represents the number of letters they missed with each eye.)
- Abnormal findings might be documented as: “20/20 -2 in left eye, 20/200 in right eye with no glasses/contact lenses.” (This reflects abnormal findings in the right eye).
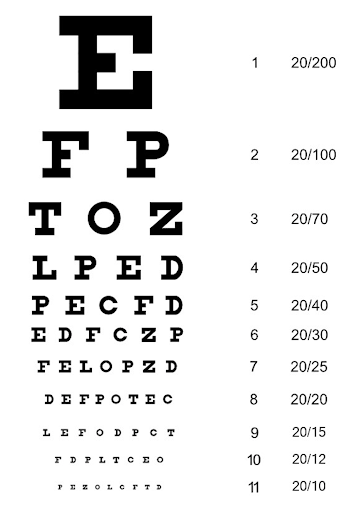
Figure 17: Snellen eye chart.
(By Khex14 – Own work, Creative Commons Attribution-Share Alike 3.0 Unported license, https://commons.wikimedia.org/w/index.php?curid=31308551)
Near vision
You should evaluate visual acuity for near vision if a client reports difficulty or if you observe potential issues. For example, you might observe a client extending their arms to hold a book far away or bringing it very close to their eyes.
There are various near vision eye charts available that have varying size numbers or letters to read (e.g., Rosenbaum pocket vision screener, Runge near card, Jaeger card, Figure 18). However, these near vision eye charts have not undergone the same kind of rigorous research as the Snellen eye chart has. Additionally, there have been reported issues such as lack of standardization in terms of font type, font thickness, and letter size progression (Cooke et al., 2019; Horton & Jones, 1997).
Nurses often conduct a basic evaluation of near vision by having the client read a newspaper or book out loud. Use the following steps:
- Ensure the environment is well-lit.
- If the client uses glasses or contact lenses for near vision, they should leave them on/in during this test.
- Ask the client to fully cover one of their eyes with the palm of their hand or an eye occluder if you have one and then, hold the reading material about 35–45 cm away from their eyes and read a couple of sentences out loud.
- Repeat step three with the opposite eye.
-
- Normally, clients can read with no blurry vision, no squinting, and no adjustment of the reading material closer or farther away from them.
- Abnormal findings may include blurry vision, squinting, and adjustment of the reading material by extending their arms or bringing it closer to them.
Figure 18: Near vision eye chart.
“111012-F-ZT401-067.JPG” by Airman 1st Class Brooke P. Beers for U.S. Air Force is in the Public Domain. Access for free at https://www.pacaf.af.mil/News/Article-Display/Article/593609/keeping-sight-all-right/
Clinical Tip
When assessing visual acuity for distance, note the line where the client can read all of the letters with a maximum of two errors.
Example 1: If the client incorrectly identifies two of the five letters on the 20/40 line, this means they were unable to correctly read all of the letters on this line except two. Thus, their visual acuity is noted as 20/40 – 2. Remember, they can make a maximum of two errors on the line where their visual acuity is noted.
Example 2: If the client can accurately read all of the letters on the 20/30 line and only 3 of the 7 letters on the next line (20/25 line), this means they made more than two errors on the 20/25 line. Thus, their visual acuity is noted as 20/30 +3. The +3 refers to the three letters they could read on the next line: the 20/25 line.
Contextualizing Inclusivity
Some clients may be unable to stand due to muscle weakness, fatigue, balance problems, or being in a wheelchair. If so, lower the Snellen eye chart so that it is located on the wall at about their eye level.
Several alternatives are available for young children or individuals who are unable to read letters, including the Tumbling E chart (Figure 19) or a chart with pictures.

Figure 19: Tumbling E chart.
(By Tigana chileshe – Own work, CC BY-SA 4.0, https://commons.wikimedia.org/w/index.php?curid=64435390).
Prioritizing Care
All abnormal findings related to visual acuity should be documented and reported to the physician or nurse practitioner. If a client has visual acuity worse than 20/30, you should refer them to an eye specialist.
However, some abnormal findings require immediate action. For example, a sudden change in vision (e.g., partial or complete loss) is a priority of care and you should immediately notify the physician or nurse practitioner.
Activity: Check Your Understanding
References
Cooke, M., Winter, P., McKenney, K., Packard, K., Williams, V., Dorsey, E., Szabo, A., Visotcky, A., Warren, C., Wirostko, W., Weinberg, D., Kim, J., & Han, D. (2019). An innovative visual acuity chart for urgent and primary care settings: validation of the Runge near vision card. Eye, 33 (7), 1104-1110. https://doi.org//10.1038/s41433-019-0372-8
Horton, J., & Jones, M. (1997). Warning on inaccurate Rosenbaum cards for testing near vision. Survey of Ophthalmology, 42(2), 169-174. https://doi.org//10.1016/s0039-6257(97)00055-6