Chapter 15 – Neurological system assessment
CN III, IV, and VI – Oculomotor, Trochlear, and Abducens Nerves
This section explores three different evaluations: assessment of the eyelids, pupillary light reflex, and extraocular eye movements.
Eyelids (specific to CN III)
- Ask the client to look straight at you and observe their eyelids.
- Normally, eyelids are open with equal palpebral fissure, which is the opening between the upper and lower eyelids. The upper eyelid crosses the iris and is positioned between the upper limbus and the pupil (the upper part of the sclera should not be visible).
- Abnormal findings include unequal palpebral fissures such as drooping of one eyelid or eyelid retraction.
- Note the findings:
- Normal findings might be documented as: “Equal palpebral fissures bilaterally.”
- Abnormal findings might be documented as: “Drooping of left eyelid” or (as shown in Figure 9) “Left eyelid retraction.”
Figure 9: Left eyelid retraction.
(By Andrewya – Own work, Public Domain, https://commons.wikimedia.org/w/index.php?curid=7028920)
Pupillary Light Reflex (specific to CN II and CN III) and Accommodation (CN III)
The pupillary light reflex assesses the eye’s response to light and innervation of CN II (optic) and CN III (oculomotor) while testing for accommodation refers to the eye’s ability to accommodate for near objects and innervation of CN III (oculomotor). Beginning with pupillary light reflex followed by accommodation, the steps in the assessment include:
- To test pupillary light reflex, have the client look straight ahead at a distant point on the wall behind you (e.g., at the opposite end of the room) to slightly dilate the pupils. If possible, also reduce the lighting in the room to dilate the pupils.
- First, assess the pupils for shape, equality, and size.
- Normally, the pupils should be round, equal in size and shape, and sized 2 to 8 mm in diameter. Normal size will depend on the ambient lighting; for example, the diameters of normal pupils are smaller in a well-lit environment (2–4 mm) and bigger in a darker environment (4–8 mm).
- Abnormal findings may include pupils that are not round, are unequal in size and shape, or are smaller or larger than the normal size.
- Ask the client to continue looking straight ahead at the distant point on the wall. Turn on your penlight. Move the light from the right side of the client to directly in front of their right eye, pause for 1–2 seconds, and then move the light back out to the side: the light should activate CN II to send a message to the brain, and then CN III should send a message to the pupillary muscles causing pupillary constriction.
When pausing the light on the eye, observe the clients’ right eye and left eye for pupillary constriction. If necessary, perform this procedure twice so that you can focus on the right eye (for direct response: meaning the pupil of the eye on the side where the light is introduced constricts), and then focus on the left eye (for consensual response: meaning the pupil of the opposite eye where the light is introduced also constricts). Repeat this step for the left eye and observe direct and consensual responses (see Video 5). Additionally, note the size of the pupil afterwards; it should return to the same size before the light was introduced.
-
- Normally, you should see a direct response and a consensual response. Normal constriction is often described as prompt or brisk, meaning it happens right away. And when you remove the light, normally, pupils will return to the same size/shape they had before you introduced the light.
- Abnormal findings include no direct and/or consensual response (the response is absent and pupils do not constrict), or when pupillary constriction is sluggish (slow).
Video 5: Pupillary light reflex test.
- To test accommodation, first have the client stare straight ahead at a distant point on the far wall and if possible, have the lights dimmed to dilate the pupils. While they are staring straight ahead, explain to the client that you are going to move your index finger (or your penlight turned off) in front of their nose and slowly bring it closer to their nose. Ask them to shift their gaze from looking at the distant point on the wall to your finger and stay focused on your finger. Next, place your index finger in front of their nose (about 20 to 30 cm from the tip of their nose and slowly move it closer so that it is about 8 cm from the tip of their nose).
- Normally, the client should shift their gaze to your finger (convergence of the eyes inward) accompanied by pupillary constriction.
- Abnormal findings include inability to shift eyes simultaneously and lack of pupillary constriction.
- Note the findings:
- Normal findings might be documented as: “Pupils round, 3 millimetres, and equal in size. Brisk, direct and consensual light reflex noted bilaterally. When testing for accommodation: pupillary constriction and convergence of eyes noted.” (In some institutions, this is sometimes noted as PERRLA: pupils equal round reactive to light and accommodation).
- Abnormal findings might be documented as: “No direct or consensual light reflex noted bilaterally.”
Clinical Tip
It can sometimes be difficult to evaluate the pupil size and pupillary constriction with clients who have dark irises. If needed, ask them to look up while doing the assessment; this can sometimes help. Alternatively, use a second penlight and shine the light tangentially to highlight the iris without causing an unintentional pupillary reflex.
Extraocular Eye Movement (specific to CN III, IV, and VI)
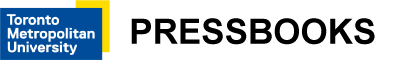
The extraocular eye movement is innervated by CN III, IV, and VI (see Figure 10).
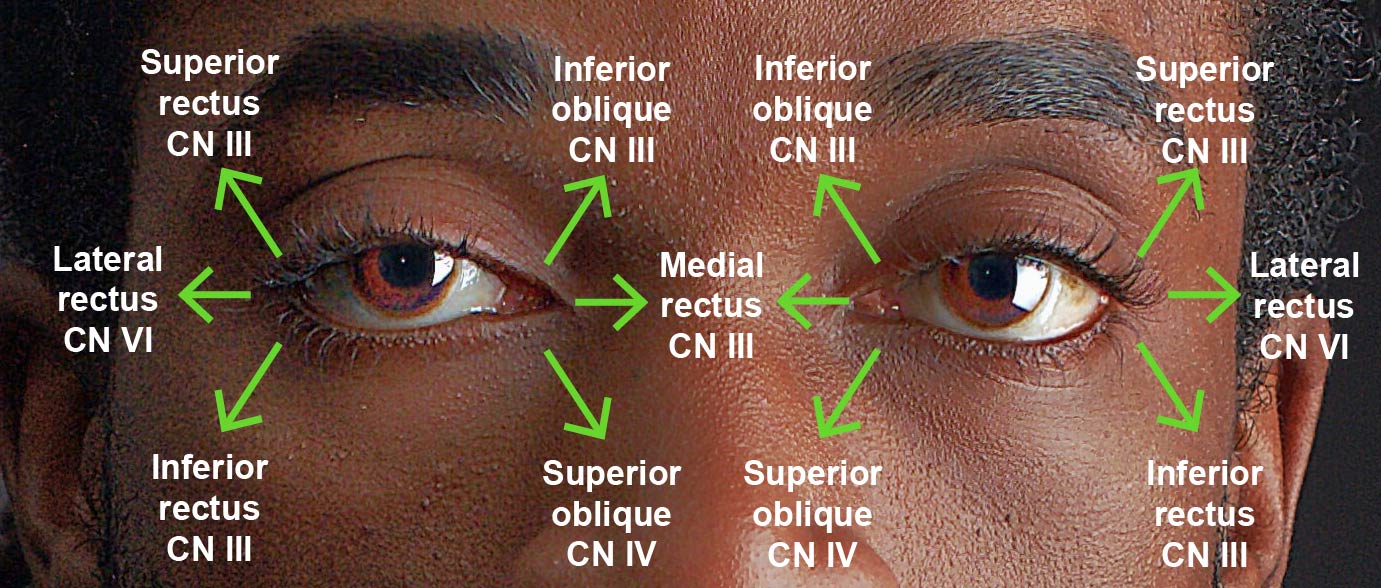
Figure 10: Extraocular movement via cranial nerves. (Illustrator Arina Bogdan)
- Sit or stand about 3 to 4 feet (or two arms lengths away from the client) at the same level.
- Ask the client to stare at your nose.
- Normally, the client’s gaze is midline.
- Abnormal findings include deviation of one of the eyes or both. The deviation may involve the eye moving inward, outward, up, or down.
- Place your index finger straight out in front of you and ask the client to keep their head still and follow your finger with their eyes through an “H” or what is also called the six diagnostic positions (see Figure 11). Positions include: diagonally in superior field, laterally at eye level, and diagonally in the inferior field. You should move your finger into each of these positions by fully extending your arm. Move back to centre each time you move to one of these positions and complete these movements on both sides. Hold your finger in each of these six positions for about two seconds. If the client moves their head, remind them to keep their head still and only follow your finger with their eyes. Ask the client if they experienced any double vision. See Video 6.
- Normally, eye movement is smooth, , with no , and no double vision.
- Abnormal findings might include disconjugate movement, nystagmus, and double vision.
- Note the findings:
- Normal findings might be documented as: “Smooth, conjugate movement with no double vision.”
- Abnormal findings might be documented as: “Disconjugate eye movement, nystagmus of left eye with extreme lateral gaze, and double vision noted by client.”
Figure 11: Six diagnostic positions for testing.
Video 6: Extraocular eye movement test.
Contextualizing Inclusivity
If the client is a sleeping infant, you should generally wait until they awake and spontaneously open their eyes before you assess pupillary light reflex. You can also have the parent or other caregiver hold the infant.
If the client is unconscious, you will need to open their eyes to assess pupillary light reflex. To do so, place the thumb pad of your non-dominant hand over the superior edge of the orbital bone and pull the eyelid up and open (see Figure 12).
 Figure 12: Opening an unconscious client’s eye to assess pupillary light reflex.
Figure 12: Opening an unconscious client’s eye to assess pupillary light reflex.
Priorities of Care
A serious finding is what is often referred to as a “blown” pupil (the pupil is fixed, unresponsive, and dilated). This condition is often associated with brain herniation, meaning the brain tissue shifts due to increased intracranial pressure. Brain herniation can be related to various pathophysiological process such as brain trauma, stroke, aneurysm, or tumour. Unilateral or bilateral fixed and dilated pupils should be immediately reported to the physician or nurse practitioner, while you stay with the client and complete a primary survey.
Anisocoria (unequal pupil size) does not require treatment unless it is new onset. Many clients have unequal pupil size, but a new onset may be of concern because it can be associated with neurological problems, stroke, infection, or eye trauma. Complete a focused assessment and report findings to the physician or nurse practitioner.
refers to eyes moving together (in unison).
is repetitive, involuntary eye movement in which the eye looks like it is quivering and can move up-down, side-to-side or in a circular motion.