Chapter 15 – Neurological system assessment
Introduction to Cranial Nerves
In total, 12 paired cranial nerves originate within the brain and brainstem and extend into multiple branches (see Figure 6).
The 12 cranial nerves are related to sensory and/or motor functions (see Table 4). Sensory refers to senses such as seeing, hearing, tasting, smelling, and touching, while motor refers to movement. Innervation and associated responsibilities of the nerves can be affected when the nerve is damaged from a physical trauma (e.g., an accident), a surgical intervention, a (related to a stroke, cerebral inflammation, tumour, aneurysm), or a condition resulting in (e.g., multiple sclerosis).
The next section explores some of the most common approaches that nurses use to examine the 12 pairs of cranial nerves. Keep in mind that there are many ways to assess cranial nerves, and an abnormal finding may indicate damage to the nerve. These findings should be considered in the context of the complete neurological examination.
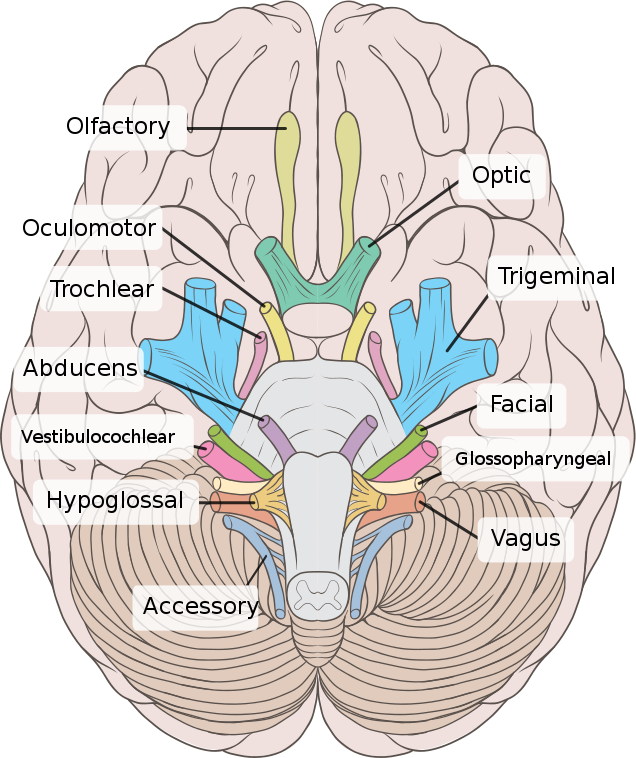
Figure 6: Cranial nerves.
(This image is licensed under the Creative Commons Attribution 2.5 Generic license and taken from https://commons.wikimedia.org/w/index.php?curid=15108118)
Table 4: Cranial nerves.
|
Nerves |
Neurological signs and symptoms (when CN is damaged) |
|
CN I (1) Olfactory nerves Sensory nerves related to smell. |
|
|
CN II (2) Optic nerves Sensory nerves related to visual acuity (how well a person’s eyes can identify shapes and details of an object at a specific distance) and visual fields (periphery of vision). This nerve is also responsible for sending a message to the brain when light is introduced to the eye when assessing pupillary light reflex to evaluate CN III. |
|
|
CN III (3) Oculomotor nerves Sensory nerves related to pupil innervation (pupillary constriction) and lens shape. Motor nerves related to upper eyelid movement and eye muscle movement specific to four muscles (superior rectus, inferior rectus, medial rectus, and inferior oblique) controlling eye movements: diagonal upward (both inward and outward); diagonal downward-outward; horizontal inward. |
|
|
CN IV (4) Trochlear nerves Motor nerves related to eye muscle movement specific to one set of muscles (superior oblique) controlling the diagonal downward-inward movement of the eye. |
|
|
CN V (5) Trigeminal nerves Sensory nerves related to the sense of touch on facial (forehead, maxillary, mandible) and the cornea. Motor nerve related to the innervation of the temporal and masseter muscles of the face. |
|
|
CN VI (6) Abducens nerves Motor nerves related to eye muscle movement specific to one set of muscles (lateral rectus) controlling the horizontal outward movement of the eye. |
|
|
CN VII (7) Facial nerves Sensory nerves related to taste on the dorsal side of the tongue on the anterior two-thirds (at the front of the tongue). Motor nerves related to movement of the facial muscles (i.e., facial expressions). |
|
|
CN VIII (8) Vestibulocochlear nerves Sensory nerves related to balance (vestibular) and hearing (cochlear). This is a set of two nerves including the vestibular nerves and the cochlear nerves (with some motor function). |
|
|
CN IX (9) Glossopharyngeal and CN X (10) Vagus nerves These nerves work together: CN IX carries afferent messages to the brain and CN X carries efferent messages to the affected area. Sensory nerves (CN IX) related to taste on the dorsal side of the tongue on the posterior third (toward the back of the tongue) Motor nerves related to movement of the soft palate, uvula, and pharynx, and some muscles of the tonsillar pillars, swallowing, and speech. |
|
|
CN XI (11) Spinal accessory nerves Motor nerves that innervates and controls the sternocleidomastoid and trapezius muscles. |
|
|
CN XII (12) Hypoglossal nerves Motor nerves related to tongue movement and strength. |
|
is an abnormal occurring area in the brain.
is a process when the myelin sheath surrounding nerves becomes damaged and is destroyed.
are areas of skin innervated by specific nerves.
refers to bilateral blinking (corneal reflex) when a stimulus is applied to the edge of the cornea.
refers to pupils that are non reactive to light.

