Chapter 16 – Vestibulocochlear System Assessment – The Ears
Otoscopic Examination
You will use an otoscope (see Figure 16) to conduct the otoscopic examination. This medical instrument has a pointed end that fits just inside the opening of the ear and provides illuminated magnification so that you can view the external ear canal and tympanic membrane.
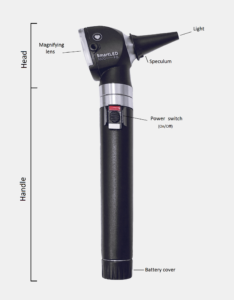
Figure 16: Otoscope.
(By Rouibi Dhia Eddine Nadjm – Own work, https://commons.wikimedia.org/w/index.php?curid=120072656 This file is licensed under the Creative Commons Attribution-Share Alike 4.0 International license.)
If the client’s ear is obstructed with earwax, you might be unable to visualize the tympanic membrane. If so, begin by cleaning the ear. The best way to do this is to place 2 to 3 drops of a warm mineral oil solution into the ear (or use 1 part hydrogen peroxide, 1 part warm water) (American Academy of Otolaryngology-Head and Neck Surgery Foundation, 2024). With the client lying on their side with the affected ear up, leave the solution in for at least 15 minutes to both soften and loosen the earwax. Next, you can use a bulb syringe with warm water to gently flush the ear over a basin or sink. Consult a physician or nurse practitioner first if the client has had ear surgery, ear infections, or perforation of the tympanic membrane (Berg, 2023).
Steps for the otoscopic examination include (see this video for an example of an otoscopic examination):
- Have the client sit on the examination table or in a high Fowler’s position. A young child may sit on a parent’s lap or in a supine position with their head turned away from you so that they are stabilized and still.
- Place a speculum cover on the otoscope and turn the otoscope light on.
- Using the hand of the same side as the ear you are inspecting (e.g., right ear, right hand), grasp the handle close to the otoscope head gently between your thumb, index finger, and middle finger (similar to how you would hold a pen).
- Ask the client to slightly tilt their head away from you and keep their head still in this position while using your opposite hand to pull the helix up and back to straighten the external canal so that you can better visualize the tympanic membrane. If the client is under 3 years of age, pull the earlobe down and slightly back instead.
- Gently insert the speculum tip just inside the external auditory meatus. Do NOT force the speculum tip in. Do NOT push the whole speculum in – only the tip.
- To stabilize the otoscope and ensure the speculum doesn’t move, you can rest the back of your hand (the one holding the otoscope) on the client’s cheek. Some healthcare professionals gently rest the speculum tip on the back of the tragus to stabilize it, which can be helpful. Otherwise, ensure the speculum touches no other parts of the ear: this can damage the ear canal and can also be very painful if the client has an ear infection.
- Look through the lens and inspect the canal for any signs of inflammation (erythema, swelling), discharge, and foreign bodies (e.g., toys, beads, pebbles, cotton from a cotton swab, or bugs such as spiders, bed bugs, flies, or earwigs). Describe the colour and quantity of earwax.
- Continue looking through the lens to inspect the tympanic membrane for colour, contour, discharge, and integrity.
- Normally, the tympanic membrane is a whitish-light grey colour, shiny and translucent resembling a stretched piece of plastic wrap, flat, with no discharge, and intact with no perforations such as holes or tears.
- Abnormal findings include:
- Discolouration. If present, note the colour. Reddened membranes are often associated with infections, yellow membranes may reflect fluid in the inner ear, and dark/black/blue membranes can be associated with hemorrhage. White patches may indicate scarring of the membrane from chronic ear infections.
- Bulging membrane. If present, note the level of bulging (mild, moderate, severe). Bulging sometimes occurs with cases of otitis media and effusion.
- Discharge. If present, note the colour (clear, sanguineous, serous, yellow, green, white) and the consistency (thin, thick).
- Perforations. If present, note the appearance and the location.
- Repeat for the other ear.
- Document the findings:
- Normal findings might be documented as: “External ear canals have no signs of erythema, swelling, discharge, or foreign bodies. Tympanic membranes are intact, pearly grey in colour, shiny, flat, with no discharge.”
- Abnormal findings might be documented as: “Bright red tympanic membrane in left ear with perforation.”
References
American Academy of Otolaryngology-Head and Neck Surgery Foundation (2024). Earwax (cerumen impaction). https://www.enthealth.org/conditions/earwax-cerumen-impaction/
Berg, S. (2023). What doctors wish patients knew about proper ear care. https://www.ama-assn.org/delivering-care/public-health/what-doctors-wish-patients-knew-about-proper-ear-care

