Chapter 1 – Introduction to Health Assessment
Priorities of Care
Why is clinical judgment important? How does it guide the provision of care?
Clinical judgment is important to ensure the nurse’s actions are based on the client’s most important needs. Clients often have several needs, and some are more important than others. As such, nurses need to assess and evaluate the priorities of care: what actions are most important to take first, and then what actions can follow. Typically, priority actions are those that prevent clinical deterioration and death.
Maslow’s Hierarchy of Needs
Priorities of care can be determined using several frameworks such as Maslow’s Hierarchy of Needs. For example, at the most basic level, life requires an open airway to breathe, the physiological process of breathing, and the circulation of blood and oxygen throughout the body. Airway, breathing, and circulation are the ABCs, which you might have learned if you have taken a cardiopulmonary resuscitation (CPR) course.
Maslow’s Hierarchy of Needs was developed to consider basic human needs and motivations of healthy individuals (Bouzenita & Wood Boulanouar, 2016; Francis & Kritsonsis, 2006; Gambrel & Cianci, 2003). Although not well known, Maslow’s work was closely influenced by the Blackfoot tribe in Canada (James & Lunday, 2014). One version includes five levels of needs: those related to physiological, safety, love, esteem, and self-actualization (Maslow, 1943), which can help prioritize care in nursing. Figure 2 presents one adapted version of Maslow’s Hierarchy.
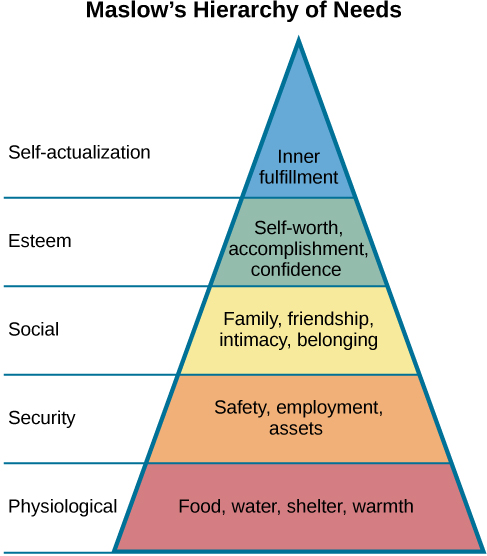
Figure 2: Maslow’s Hierarchy of Needs (see attribution statement at bottom of page)
Drawing upon this framework, a nurse can use health assessments to explore five levels of needs:
- Physiological needs – fundamental physical needs required for survival such as air, food/drink, sleep, warmth/clothing/shelter.
- Are these basic physiological needs being met? Is the client’s breathing and circulation supported?
- Safety – needs related to a secure physical and emotional environment.
- Does the client feel safe and secure in general in life? Does the client feel safe and secure in the healthcare environment? Is the bed lowered to the lowest position when you finish your assessment? Is the call bell in reach?
- Love and belongingness – needs related to relationships including friendship and family, intimacy and affection, work, and trust and acceptance.
- Does the client feel love and belongingness in general in their relationships? More specifically, does the client feel cared for by nurses and other healthcare providers?
- Esteem – feelings related to self-worth, dignity, respect, and achievement.
- Does the client feel respected and valued in general by others? Does the client feel respected and valued within the healthcare environment?
- Self-actualization – a process or action of reaching one’s full potential and self-fulfillment.
- What is important to the client in terms of what they want to achieve in life in general? What are the client’s goals that they may have for themselves in their own health and healing journey? Does the client feel satisfied, confident, and accomplished?
You can use Maslow’s Hierarchy of Needs as a guide, but it is important to be aware of the critiques and possible limitations in its application. See Video 1 of a conversation between Dr. Lisa Seto Nielsen and Mahidhar Pemasani.
Video 1: A discussion about Maslow’s Hierarchy of Needs
Criticisms of Maslow’s hierarchy are related to it being ethnocentric, based on individualistic societies, and not necessarily taking into account diversity in culture, gender, and age (Bouzenita & Wood Boulanouar, 2016; Francis & Kritsonsis, 2006; Gambrel & Cianci, 2003). It should not be arbitrarily applied to all healthcare encounters. Although you may initially focus on physiological needs to ensure the client is stable, the client may have different priorities that are more important to them. By drawing upon Indigenous knowledge, it is vital to recognize the role of community and advocacy in reaching self actualization at every level (Bennett & Shangreaux, 2005). This is particularly important in the context of systemic racism and oppression and the existing disparities among racialized populations including Black communities and Indigenous People.
Levels of Priority of Care
Because of the importance of recognizing clinical deterioration in a client, a nurse must always be attuned to the set of physiological needs that are important to maintain life and prevent death. These priorities of care are related to the ABCs – airway, breathing, and circulation – introduced above. These priorities of care are often categorized as first, second, or third level, with the first level taking a priority (see Table 3).
Table 3: Priorities of care
|
Priority of care |
Examples |
|---|---|
|
First-level priority of care are problems/issues that reflect critical findings, clinical deterioration and/or are life-threatening – and therefore require urgent action. Urgent means that action must be taken immediately. |
A client in respiratory distress as evident by , nasal flaring, laboured breathing, , and decreasing oxygen levels or a client with such as chest pain or the absence of or decreasing pulse or blood pressure. |
|
Second-level priority of care are problems/issues that may lead to clinical deterioration and may become life-threatening without intervention – and therefore require prompt action. Prompt means that action must be taken quickly. |
A client with signs and symptoms such as: altered level of orientation, decreased level of consciousness/confusion, elevated temperature, increasing pain levels, and cold extremities. This may include a client with a head injury who can deteriorate quickly in some cases. You should assess if they experienced a loss of consciousness and have any associated symptoms with a concussion. |
|
Third-level priority of care are problems and issues that are typically focused on functional health, client education, and counselling. These should be addressed, but they are non-urgent and can wait until the client is stable. The problem/issue is not acute in nature, but intervention is required to support the client’s activities of daily living, their knowledge level, and their mental health and wellbeing |
A client who is post-operative and requires assistance with hygiene and mobility, a client who reports increasing stress levels and problems sleeping, or a client who is newly diagnosed with diabetes and requires education around nutrition and monitoring their blood glucose levels. |
With regard to levels of care, it is essential to consider what is most important to the client. You should treat the client as the expert in their own life – and also as the expert in decisions about their own healthcare, if they choose. Although a client may have plummeting blood pressure, you need to consider tailoring the intervening action to their wishes. Some clients may not wish for intervention in a life-threatening circumstance. Therefore, you always need to be open to the client’s wishes, but also consider whether they are able to weigh the consequences of their decision (i.e., are they competent to consent?).
Urgent Priorities of Care: Mental Health
In practice, mental health is typically not categorized as a first- or second-level priority of care unless the client is showing signs of clinical deterioration based on the examples noted in Table 3. In some situations, mental health may be positioned as a third-level priority of care, for example when a client is experiencing anxiety, depression, grief, but shows no signs of suicidal ideation. These symptoms should be addressed, but according to this framework, they are considered less urgent compared to first- and second-level priorities of care. However, sometimes, you should think differently about how mental health is a priority of care.
In some situations, mental health may take precedence. For example, a client who has attempted suicide or has just overdosed will probably have other physical symptoms as a result and therefore require urgent intervention and constant observation as per Table 3. However, the descriptions of the priorities of care presented in the table do not account for a client who has voiced a specific plan for suicide and has identified when and how. This client is at very high risk and requires urgent intervention regardless of what may be viewed as their physical health state or history. The description of priorities of care listed above does not account for this except as a third-level priority – but a client with suicide ideation or has voiced wanting to hurt others requires urgent action to protect their own wellbeing and others and the possibility of clinical deterioration as a result of their actions.
Intervention Types
As illustrated by the text box above, you will need to use your own judgement to determine how to act when a cue presents itself and how to categorize these interventions. This could involve four general types of interventions that you need to be aware of (see Table 4) including effective, ineffective, unrelated, and contraindicated. These types of interventions will become more clear as you begin to learn about normal, abnormal, and critical findings for various body systems, and how interventions and actions will affect these findings and the client.
Table 4: Types of interventions
|
Type of Intervention |
Example The client has no pulse, their chest is not rising, and they are not responsive. As a nurse you need to make a clinical judgment on how to act based on these cues. |
|---|---|
|
Effective (or indicated) interventions are actions that are adequate to produce the intended result and help the client. |
Begin CPR immediately. This is also an evidence-informed intervention because a delayed response results in poor outcomes as per the research. |
|
Ineffective interventions are actions that are not adequate to produce the intended result and therefore will not help the client. |
Provide mouth-to-mouth resuscitation; without compressions, the oxygen will not circulate. |
|
Unrelated (or non-essential) interventions are actions that will not produce an effect (positive or negative) and therefore will not help the client. |
Notify the client’s employer. |
|
Contraindicated interventions are actions that are not recommended because they have the potential to cause harm to the client. |
A contraindicated intervention is to delay resuscitation until a physician is present. |
Activity: Check Your Understanding
Attribution statement for Figure 2
Authors: Spielman et al. Publisher/website: OpenStax Book title: Psychology 2e. Publication date: Apr 22, 2020 Location: Houston, Texas. Book URL: https://openstax.org/books/psychology-2e/pages/1-introduction Section URL: https://openstax.org/books/psychology-2e/pages/1-2-history-of-psychology. Textbook content produced by OpenStax is licensed under a Creative Commons Attribution License 4.0 license.
References
Bennett, M., & Shangreaux, C. (2005). Applying Maslow’s Hierarchy Theory. First Peoples Child & Family Review: a Journal of Innovation and Best Practices in Aboriginal Child Welfare Administration, Research, Policy & Practice, 2(1)89-116. https://doi.org/10.7202/1069540ar
Bouzenita, A. I. & Wood Boulanouar, A. (2016). Maslow’s hierarchy of needs: An Islamic critique. Intellectual Discourse, 24(1), 59-81.
Francis, N.H. & Kritsonis, W.A. (2006). A brief analysis of Abraham Maslow’s original writing of self-actualizing people: A study of psychological health. Doctoral Forum: National Journal of Publishing and Mentoring Doctoral Student Research, 3(1), 1-7.
Gambrel, P., & Cianci, R. (2003). Maslow’s hierarchy of needs: Does it apply in a collectivist culture. The Journal of Applied Management and Entrepreneurship, 8(2), 143–161.
James, A., & Lunday, T (2014). Native birthrights and Indigenous science. Reclaiming Children and Youth, 22(4), 56-58.
Maslow, A. (1943). A theory of human motivation. Psychological Review, 50(4), 370-396. https://doi.org/10.1037/h0054346
is rapid respiratory rate.
are when the intercostal muscles are pulled inward when breathing.
a clinical state in which circulatory perfusion is compromised.