Chapter 12 – Peripheral Vascular System Assessment
Subjective Assessment
Subjective assessment of the peripheral vascular system (PVS) involves asking questions about the health of the client and symptoms that occur because of pathologies that affect the vasculature of the body. A full exploration of these pathologies is beyond the scope of this chapter, but common problems associated with this system include (PVD), , , , , and .
Knowledge Bites
Many peripheral vascular symptoms are related and are caused by the same issue. See Table 2 for the signs and symptoms of arterial and venous issues and watch Video 1:
Video 1: Arterial and venous issues [5:00]
Peripheral arterial issues occur when there is a problem with perfusion (blood flow is restricted or blocked) in the arteries due to a blockage. This can be caused by atherosclerosis (narrowing of the arteries caused by plaque build up on the arterial walls) and arteriosclerosis (hardening, stiffening and loss of elasticity of the arterial walls); these are both forms of peripheral arterial disease. When blood flow is restricted, oxygen and nutrients are not efficiently delivered to body tissues. When tissues in the periphery do not get sufficient oxygen-rich blood, hypoxia can develop, leading to pain, numbness, ulcers, fatigue, and other symptoms and signs. However, it’s important to note that many clients with arterial disease don’t have symptoms, so your assessment of risk factors is important.
Peripheral venous issues are related to venous insufficiency: veins in the periphery (typically the legs) restrict the return of blood to the heart, causing venous stasis (collection or pooling of blood) in the peripheral limbs (typically the feet and lower legs). This is often caused when the one-way venous valves are not working properly and allow backflow of blood, as opposed to the forward movement of blood. It can also be caused by blood clots. and varicose veins can arise secondary to venous insufficiency and venous stasis (Anwar et al., 2021). Varicose veins (see Figure 4) are dilated, bulging, and twisted veins that can be superficial (observed on the skin’s surface) or deep within the leg and not visible upon inspection. You may hear the term tortuous veins, which refers to twisted veins. Varicose veins can have a genetic component and can also have primary causes that are relatively unknown (Anwar et al., 2021). Some varicose veins are painful and depending on the associated cause may result in blood clots. Another venous issue is spider veins (Figure 5), which appear as small flat dark red, blue, or purple venous patterns close to the surface. Spider veins can cause body image issues, but they are not painful and are not related to serious problems such as blood clots.
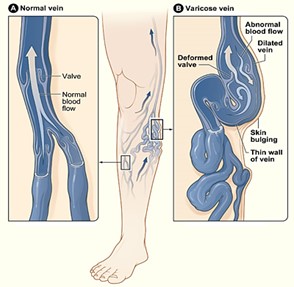
Figure 4: Comparison of a normal and varicose vein.
(Attribution: Photo by National Heart Lung and Blood Institute. – Varicose veins., Public Domain, https://commons.wikimedia.org/w/index.php?curid=6885995)

Figure 5: Spider veins.
Table 2: Venous and arterial issues signs and symptoms.
| Venous issues | Arterial issues |
|
NOTE: Another type of ulcer is a diabetic ulcer typically found on the plantar side of the foot. Although they resemble arterial ulcers, their underlying pathophysiology is related to the effects of diabetes (damage to nerve endings and vasculature and decreased sensation in feet).
|

Figure 6: Chronic venous insufficiency and venous ulcer.
(Attribution: Photo by Ashashyou – Own work, CC BY-SA 4.0, https://commons.wikimedia.org/w/index.php?curid=122884459)

Figure 7: Arterial ulcer PVD.
(Attribution: Photo by Jonathan Moore – Creating the Ideal Microcosm for Rapid Incorporation of Bioengineered Alternative Tissues Using An Advanced Hydrogel Impregnated Gauze Dressing: A Case Series. The Foot and Ankle Online Journal 1 (9): 2., CC BY 3.0, https://commons.wikimedia.org/w/index.php?curid=6886430)
Common symptoms that can be related to the PVS include pain-related sensations, numbness, changes, skin temperature changes, edema, and ulcers. See Table 3 for guidance on the subjective health assessment. Many of the questions in the table align with the PQRSTU mnemonic, but you should probe symptoms in the order of relevance, as opposed to sequentially with the PQRSTU mnemonic.
Ask about any medications the client is taking: name, dose, frequency, reason it was prescribed, and how long they have been taking it.
Also ask questions focused on health promotion. Depending on the context, you may ask these questions and engage in a discussion during a subjective assessment or after an objective assessment. A section on “Health Promotion Considerations and Interventions” is included later in this chapter after the discussion of objective assessment.
Table 3: Guidance on subjective assessment.
|
Symptoms |
Questions |
Clinical tips |
|
Pain-related sensations such as sharp pain, sensitivity, cramping, achiness, and numbness in the legs/feet and/or arms/hands. These types of sensations are common with perfusion issues and more often affect the lower limbs. These sensations worsen as circulation is reduced. Arterial perfusion issues usually lead to sharp pain and cramping in the lower legs and feet, as well as numbness and sensitivity in the feet and toes. Pain-related sensations with venous issues often include achiness and a heavy feeling. |
Do you currently have or have you recently had any pain, discomfort, tenderness, numbness, sensitivity, and cramping in your feet or legs? Additional probes if the response is affirmative: Region/radiation: Where is the pain located? Does it move around, or do you feel it anywhere else Quality/quantity: Can you describe what it feels like? How bad is it? Severity: Can you rate it on a scale of 0 to 10, with 0 being no pain and 10 being the worst pain you have had Provocative/palliative: What makes it better? What makes it worse? Is it brought on by activities such as walking? If so, how long can you walk before the pain begins? Have you noticed a reduction in the amount of activity that you can do before the pain begins? Timing/treatment: When did the pain begin? Does it begin suddenly or gradually? Is it constant or intermittent? If intermittent, how long does it last for? Does it occur at night when you are in bed? Have you tried treating it with anything? Understanding: Do you know what is causing it? What do you think is causing it? |
Use the client’s words when probing. For example, they may refer to sensations as “tenderness” or “pain.” Claudication is a type of pain that happens with activity and is caused by lack of oxygen to the tissues. It is typically related to arterial insufficiency and can be felt in the feet, buttocks, calves, and thighs. This type of pain is often relieved with rest. For example, it may be an intermittent pain that subsides within ten minutes when the client rests. It is important to assess how much activity it takes to produce the pain and whether the amount of activity that exacerbates the pain has changed recently. Pain-related sensations may have a peripheral vascular or musculoskeletal or neurological cause. If you suspect peripheral vascular issues, you should assess impact on circulation: skin temperature and distal pulses (more information is provided later in the objective assessment section). Numbness and tingling sensations can be neurological-related as a result of damage to or pressure on the peripheral nerves. |
|
Skin discolouration and skin temperature changes in the distal portions of the limbs. PVD can cause changes in skin colour (cyanosis, erythema, pallor) and skin temperature (coolness, warmness). |
Have you noticed any changes in skin colour or skin temperature in your legs or arms? If the answer is affirmative, ask the client to describe the change. Additional probes if the response is affirmative: Region/radiation: Where is it located? Is it anywhere else? Quality/quantity: Can you describe what it looks like or feels like? How bad is it? Provocative/palliative: What makes it better? What makes it worse? Timing/treatment: When did you notice it? Is it constant or intermittent? If intermittent, how long does it last for? Have you tried treating it with anything? Have you sought treatment for it? Is it affected by position change (e.g., standing all day or elevating your feet? Is it worse at the end of the day? Understanding: Do you know what is causing it? |
The type of change in skin colour and temperature change can help you determine whether this is an arterial or venous issue. As a reminder, see Table 3 above for skin changes associated with arterial and venous issues. Gangrene is the death of tissue. It can occur when tissue does not receive oxygen supply as a result of occlusion in the arterial vasculature. It can happen in any part of the body but when associated with peripheral arterial disease, it is usually first observed in the toes, feet and lower limbs. The skin becomes darker in colour and can have shades of dark green and black. Gangrene requires immediate treatment to prevent further tissue damage. Sometimes amputation is required with advanced gangrene. |
|
Edema is swelling that occurs from excess fluid in the interstitial space. It is sometimes described as a heavy feeling by clients. It is most easily noticed in peripheral locations such as the feet and legs because gravity pulls the fluid downward into these dependent positions, but it may also be observed in the sacrum, abdomen, hands, and arms. Dependent edema is a type of edema that is worse while standing or when the legs/feet are below the heart level and improves when legs/feet are elevated (i.e., when lying down with legs/feet above the heart level). A common cause of peripheral edema in the older population is venous insufficiency, which is associated with dependent edema. |
Have you noticed any swelling or puffiness in your feet or ankles (or any other areas)? Have you noticed that your shoes fit more tightly? Additional probes if the response is affirmative: Region/radiation: Where is the swelling? Have you noticed it anywhere else? Timing: When did the swelling begin? Is it worse at a particular time of day? Provocative/palliative: Does anything make the swelling worse? Does anything make it better? Is it affected by position change (e.g., when standing or when legs are elevated)? Is it worse when you have been standing for a long period? Other: Have you noticed any associated colour changes to the skin? Do you have difficulty walking? Have you noticed any skin ulcers on your feet or legs? Have you noticed any recent and rapid weight gain (e.g., in the last week)? |
Assess the timing of the edema: is it acute or chronic and is it unilateral or bilateral? This will help you focus your questioning. If it is acute and unilateral, it may be a localized issue such as (DVT) or an injury. If it is chronic, it is more likely to be a systematic issue. Bilateral edema can also be associated with venous insufficiency. that is not well controlled can also cause bilateral edema due to vascular damage caused by high blood glucose levels, resulting in reduced blood circulation. Edema and rapid weight gain are sometimes related. Rapid weight gain can be suggestive of increased fluid retention (leading to edema) and is often associated with heart failure. A 2–3 lb (0.9– 1.3 kg) weight increase in 24 hours is a cue that requires immediate action. Compression stockings are often prescribed for leg edema. These are fitted elastic stockings that apply a certain amount of pressure to the leg. When leg edema is associated with venous insufficiency, it is often recommended to elevate legs and feet. These therapeutic treatments help improve blood flow and prevent pooling of blood in the legs. |
|
Ulcers are open sores on the skin. Initially, these sores are often caused by an injury to the skin, even a minor injury. They are slow to heal. Because ulcers are open to the air, they can act as an entry point for bacteria and can become infected and increase in size. |
Have you noticed any sores on your legs or feet that are slow to heal? Additional probes if the response is affirmative: Region/radiation: Where are they located? Have you noticed them anywhere else? Quality: What do they look like? Is the sore open? Are the sores wet or dry? Do you notice a discharge? If so, what colour is it? Timing: When did the sore begin? Do you know how it developed? Treatment: Have you treated it with anything? Understanding: Do you know what is causing it? |
When a client reports a leg ulcer, it is important to perform a focused peripheral vascular assessment including an objective assessment. Leg ulcers that are slow to heal are often related to peripheral venous disease. Other causes include peripheral arterial disease and diabetes. Your assessment will help you determine the type of ulcer and assess the risk for infection. |
|
Other peripheral vascular related symptoms can include fatigue, weakness, hair loss on legs, shiny skin, and erectile dysfunction. |
Have you experienced fatigue? (Ask about weakness, hair loss on the legs, shiny skin, erectile dysfunction). Use variations of the PQRSTU mnemonic to assess these symptoms further if the client’s response is affirmative. |
These symptoms can be related to other body systems and non-peripheral vascular issues. If you suspect a PVD, it is important to do a focused assessment. |
|
Personal and family health history of PVD, , high blood pressure, hypercholesterolemia, and diabetes. Each of the above conditions are risk factors for PVD. Coronary artery disease and PVD occur as a result of atherosclerosis. |
Do you have any chronic conditions or diseases (e.g., personal and/or family health history of PVD, coronary artery disease, high blood pressure, hypercholesterolemia, or diabetes)? Is there a familial history of any of these conditions or diseases? If the client’s response is affirmative, begin with an open-ended probe: Tell me about the condition/disease? Other questions might include: Timing: When did you begin experiencing symptoms related to this condition? When were you diagnosed? Are the symptoms constant or intermittent? Quality/quantity: How does it affect you? What symptoms do you have? How bad are the symptoms? Treatment: How is it treated? Has this treatment helped? Have you had any surgeries? Do you take medication? If so, is the medication effective or do you experience any side effects? Provocative/palliative: Is there anything that makes it worse? Is there anything that makes it better? Other: Tell me about living with this condition? |
The biological and non-biological nature of family may be important to explicate when asking questions, considering that the risk factors may be influenced by genetics and/or culture. These assessment questions will allow you to gain a better understanding of the client and relevant nursing interventions and education. Although there is a genetic role to some PVDs, it is also important to consider culture in terms of family traditions and practices which can have a large role to play (e.g., eating habits, activity/exercise, smoking). Some cases of high cholesterol may involve a genetic component. Familial hypercholesterolemia is an inherited condition (the gene is present at birth) that leads to hypercholesterolemia (high levels of cholesterol in the blood) and increases the risk of atherosclerotic plaque buildup. |
Contextualizing Inclusivity
The risk of PVD increases with age, particularly for those over the age of 50. Risk factors include sedentary lifestyle, physical inactivity, obesity, high blood pressure, high cholesterol, diabetes, smoking, and diets high in saturated and trans fat, red meat, sodium, and sugar.
While assessing and responding to these risk factors, always use an inclusive approach in conducting your subjective health assessment. Inclusive health assessments should be grounded in social justice: uphold the humanity of all clients in all aspects of care, regardless of their race, ethnicity, gender, sexuality, age, ability, health decisions, and any other factors that makes them who they are. Treat everyone with dignity and recognize that each client is a human being with unique health experiences. Be aware of your biases and use a non-judgemental approach to interviewing.
Priorities of Care
All abnormal symptoms need to be explored and followed up by an objective assessment.
New onset or worsening pain-related symptoms, changes in skin colour and skin temperature, edema, and ulcers need to be fully assessed and reported to the physician or nurse practitioner. Prompt intervention is required with rapid weight gain in a short period of time (e.g., 2–3 lb or 0.9–1.3 kg in 24 hours). These issues should be reported to the physician or nurse practitioner.
With regard to arterial issues, you should be attentive to signs and symptoms that may indicate acute ischemia to the limbs: this is a decrease in peripheral perfusion that could threaten the viability of the affected limb. These signs and symptoms should be monitored and reported to the physician or nurse practitioner; they are often referred to as the 5 Ps (Obara et al., 2022):
- Pain (this could be acute pain in the affected limb and extremity that gets progressively worse).
- Pallor (extremities that become paler than the client’s normal skin colour in the affected limb).
- Pulselessness (absent pulses in the affected limb).
- Paresthesia (decreased sensation in the affected limb or a tingling or a numbness sensation).
- Paralysis (inability to move the affected limb).
Additionally, reports of gangrenous tissue (Figure 8) require prompt intervention and should be reported to the physician or nurse practitioner.

Figure 8: Gangrene: By Dr. Andreas Settje – This Picture was copied under GFDL from the german PflegeWiki., CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=168739
Activity: Check your Understanding
References
Anwar, M., Georgiadis, A., Shalhoub, J., Lim, C., Gohel, M., & Davies, A. (2012). A review of familial, genetic, and congenital aspects of primary varicose vein disease. Circulation: Cardiovascular Genetics, 5(4), 460-466. https://doi.org/10.1161/CIRCGENETICS.112.963439
London, N., & Donnelly, R. (2000). Ulcerated lower limb. BMJ, 320(7249), 1589-1591. https://doi.org.10.1136/bmj.320.7249.1589
Obara, H., Matsubara, K., & Kitagawa, Y. (2018). Acute limb ischemia. Ann Vasc Dis, 11(4), 443-448. https://doi.org.10.3400/avd.ra.18-00074
Vivas, A., Lev-Tov, H., & Kirsner, R. (2016). Venous leg ulcers. Ann Intern Med, 165(3), ITC17-ITC32. https://doi.org.10.7326/AITC201608020
refer to a group of diseases that affect the arteries and veins in the arms, legs, and abdominal area.
is a build up of plaque on the arterial walls.
refers to arteries that become hard and stiff, and thus less elastic.
is a collection or pooling of blood in the veins typically in the legs.
are dilated, bulging, and twisted veins that can often be observed on the skin’s surface and can also be deep within the leg and not visible.
open sores.
refers to high blood pressure in the veins.
or edema refers to swelling that occurs from excess fluid in the interstitial space.
refers to an indentation that remains after applying pressure over the location.
is the bony prominence on each side of the ankle.
refers to decreasing in size or commonly referred to as wasting.
is the death of tissue that can occur when there is insufficient oxygen supply.
refers to a change in colour from the person's natural skin colour.
is the formation of a blood clot in one of the deep veins, usually a leg.
is a disease that affects insulin production or effective use of insulin, a hormone required to regulate blood glucose (sugar).
is a disease that affects the coronary arteries (the arteries that deliver blood to the heart muscle). It involves narrowing or blockage of the arteries, often caused by atherosclerosis.

