Chapter 11 – Cardiovascular System Assessment
The Heart
Assessment of the heart involves inspection, palpation, and auscultation. Always begin with inspection, unless there is an immediate concern to move to auscultation or you suspect clinical deterioration.
The assessment must be performed on skin and never over clothing. You may ask the client if they would like someone present for the exam; some clients may not feel comfortable exposing their chest area and may prefer the presence of a friend, family member, or another healthcare provider.
You should always explain what you are doing and ask permission to touch. Always ensure the client’s privacy. Close the door and curtains and provide appropriate draping, considering that some of the assessment involves exposing parts of the chest. Draping should be provided to clients of all genders and ages.
The assessment is typically performed in a supine position with the client’s head on a pillow. This positioning also facilitates draping and easier landmarking, particularly with a client who has larger breasts that will need to be repositioned to expose assessment areas. For example, repositioning will be easier as larger breasts typically shift laterally in a supine position. You can ask the client to shift their breast tissue laterally and up or down as needed; if the client is unable to do so, you can ask permission to reposition their breast. In this case, always use the ulnar (outside) surface of your hand, as opposed to a grasping or cupping movement.
Clinical Tips – Landmarking the Heart
When performing an objective assessment, you will need to physically landmark several locations on the chest to inspect and palpate the precordium, palpate the apical impulse, and auscultate the apical pulse and cardiac valves. See Figure 5 and Video 5. The physical location where you assess is not always aligned with the anatomical location. For example, auscultation of cardiac valves corresponds with the direction of blood flowing out of the valve as opposed to where the valve is anatomically located.
2nd Intercostal space at right sternal border: Location of where the aortic valve is best heard because the flow of blood out of the valve is directed toward this area. This is also the location of the base of the heart.
2nd Intercostal space at left sternal border: Location of where the pulmonic valve is best heard because the flow of blood out of this valve is directed toward this area. This is also the location of the base of the heart.
5th Intercostal space at left sternal border (or 4th intercostal space in a child): Location of where tricuspid valve is best heard because the flow of blood out of this valve is directed toward this area. Note that in a child, this is located at the fourth intercostal space. Some practitioners assess the 4th intercostal space even in adults. Keep in mind that sound travels.
5th Intercostal space, left midclavicular line or just medial to the midclavicular line (or 4th intercostal space in a child): Location of where the mitral valve is best assessed because the flow of blood out of this valve is directed towards this area (the mitral valve is also called the bicuspid valve). This location is also considered the apex of the heart because it is where maximum impulse against the chest wall occurs as a result of systolic contraction of the left ventricle. Additionally, it is where the apical impulse and apical pulse are assessed.
Left sternal border: Location between the 2nd and 5th intercostal space close to the left sternal border.
NOTE: Certain pathophysiological processes will modify these locations. For example, an enlarged heart or congenital disorders may affect the anatomy of the heart and/or the location of the heart.
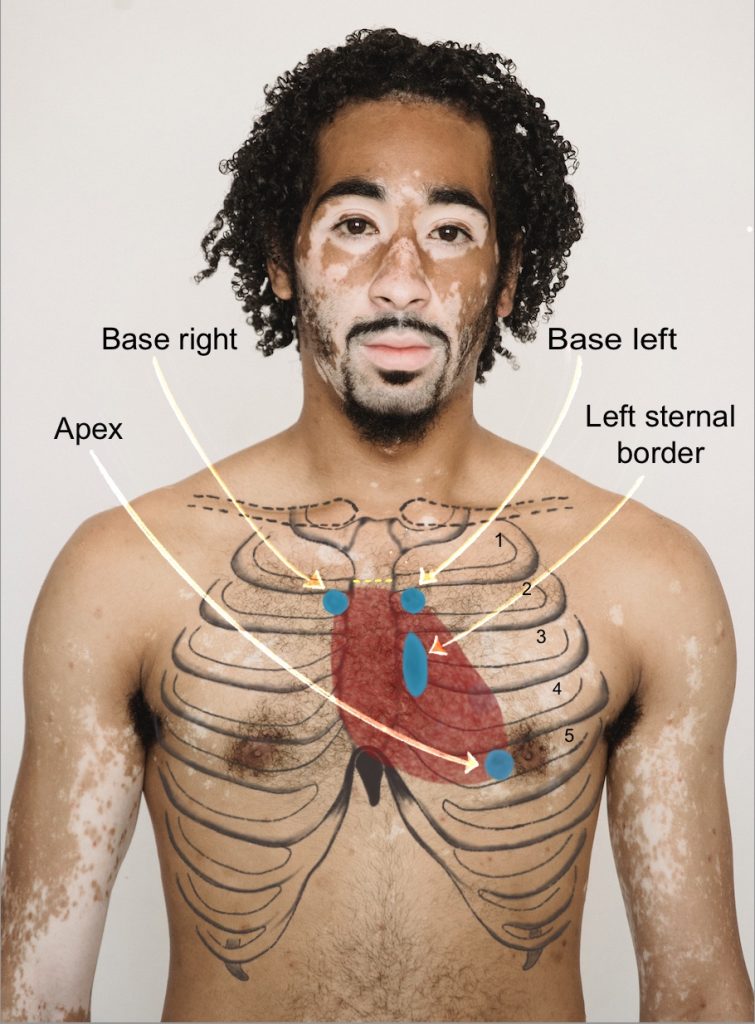
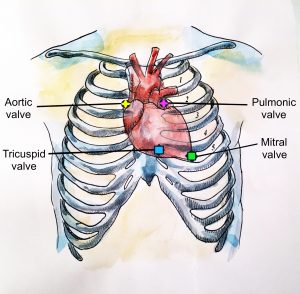
Figure 5: Landmarks
Image on left side: Photo by Armin Rimoldi from Pexels (image was cropped and illustrated upon for the purposes of this chapter)
Image on right side: Illustration by Hillary Tang from vital signs chapter (image was cropped and illustrated upon for the purposes of this chapter)
Techniques for landmarking on adults:
- There are approaches that you can begin with. The first approach is: Place your fingertips on the manubrium and slide your fingers down to the sternal angle. You will have reached the sternal angle when you feel a small ridge. The sternal angle is attached to the second rib. Slide your fingers over to the rib on the right sternal border and slide your fingers down into the space below the second rib – this is the 2nd intercostal space. This location is considered the base of the heart and where the aortic valve is best assessed. The alternative approach is: On the right side, place your index and middle fingers on the clavicle, slide down until you feel the first rib. Then, slide them into the 1st intercostal space and down over the second rib. Then, slide fingers down into the 2nd intercostal space at the right sternal border. This location is considered the base of the heart and where the aortic valve is best assessed.
- Follow this same space across the sternum into the 2nd intercostal space of the left sternal border. This location is considered the base of the heart and where the pulmonic valve is best heard.
- Now slide your fingers down the chest wall feeling for each rib and each intercostal space below the rib until you reach the 5th intercostal space at the left sternal border. This is the location of where the tricuspid valve is best heard. Stay close to the sternum because the ribs are easier to feel.
- Follow the 5th intercostal space out to the left midclavicular line or just slightly medial. This is the location of the apex of the heart, the location where you palpate the apical impulse, and the location where you auscultate the apical pulse and the mitral valve.
Video 5: Landmarking the heart.
Activity: Check Your Understanding

