Chapter 7: Vital Signs
Pulse
What is Pulse?
Pulse refers to a pressure wave that expands and recoils the artery when the heart contracts/beats. It is palpated at many points throughout the body. The most common locations to accurately assess pulse as part of vital sign measurement include radial, brachial, carotid, and apical pulse as shown in Figure 3. The techniques vary according to the location, as detailed later.
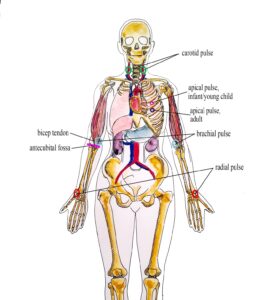
Figure 3: Radial, brachial, carotid and apical pulse (Illustration credit: Hilary Tang)
The heart pumps a volume of blood per contraction into the aorta. This volume is referred to as stroke volume. Age is one factor that influences stroke volume, which ranges from 5–80 mL from newborns to older adults.
Pulse is measured in beats per minute, and the normal adult pulse rate (heart rate) at rest is 60–100 beats per minute (OER #1, OER #2). Newborn resting heart rates range from 100–175 bpm. Heart rate gradually decreases until young adulthood and then gradually increases again with age (OER #2). A pregnant women’s heart rate is slightly higher than her pre-pregnant value (about 15 beats). See Table 3.1 for normal heart rate ranges based on age.
Table 1: Heart Rate Ranges
| Age | Heart rate (beats per minute) |
|---|---|
| Newborn to one month | 100–170 |
| One month to two years | 90–160 |
| Age 2–6 years | 70–150 |
| Age 7–11 years | 60–130 |
| Age 12–17 years | 50–110 |
| Adult and older adult | 60–100 |
Points to Consider
The ranges noted in Table 3.1 are generous. It is important to consider each client and situation to determine whether the heart rate is normal. For example, heart rate is considered in the context of a client’s baseline heart rate. The healthcare provider also considers the client’s health and illness state and determinants such as rest/sleep, awake/active, and presence of pain. You can expect higher pulse values when a client is in a stressed state such as when crying or in pain; this is particularly important in the newborn. It is best to complete the assessment when the client is in a resting state. If you obtain a pulse when the client is not in a resting state, document the circumstances (e.g. stress, crying, or pain) and reassess as needed.
Why is Pulse Measured?
Healthcare providers measure pulse because it provides information about a client’s state of health and influences diagnostic reasoning and clinical decision-making.
Tachycardia
Tachycardia refers to an elevated heart rate, typically above 100 bpm (OER #2) for an adult. Developmental considerations are important to consider, such as higher resting pulse rates in infants and children. For adults, tachycardia is not normal in a resting state but may be detected in pregnant women or individuals experiencing extreme stress (OER #2). Tachycardia can be benign, such as when the sympathetic nervous system is activated with exercise and stress. Caffeine intake and nicotine can also elevate the heart rate. Tachycardia is also correlated with fever, anemia, hypoxia, hyperthyroidism, hypersecretion of catecholamines, some cardiomyopathies, some disorders of the valves, and acute exposure to radiation (OER #2).
Bradycardia
Bradycardia is a condition in which the resting heart rate drops below 60 bpm (OER #2) in adults. In newborns, a resting heart rate below 100 bpm is considered bradycardia. However, a sleeping neonate’s pulse may be as low as 90 bpm. People who are physically fit (e.g., trained athletes) typically have lower heart rates (OER #2). If the client is not exhibiting other symptoms, such as weakness, fatigue, dizziness, fainting, chest discomfort, palpitations, or respiratory distress, bradycardia is generally not considered clinically significant (OER #2). However, if any of these symptoms are present, this may indicate that the heart is not providing sufficient oxygenated blood to the tissues (OER #2). Bradycardia can be related to an electrical issue of the heart, ischemia, metabolic disorders, pathologies of the endocrine system, electrolyte imbalances, neurological disorders, prescription medications, and prolonged bedrest, among other conditions (OER #2). Bradycardia is also related to some medications, such as beta blockers and digoxin.
Points to Consider
It is vital that healthcare providers assess clients with tachycardia or bradycardia to determine whether the findings are significant and require intervention.
Part of this content was adapted from OER #2 (as noted in brackets above):
© Apr 10, 2017 OpenStax Anatomy and Physiology. Textbook content produced by OpenStax Anatomy and Physiology is licensed under a Creative Commons Attribution License 4.0 license. Download for free at http://cnx.org/contents/7c42370b-c3ad-48ac-9620-d15367b882c6@12
Part of this content was adapted from OER #1 (as noted in brackets above):
© 2015 British Columbia Institute of Technology (BCIT). Clinical Procedures for Safer Patient Care by Glynda Rees Doyle and Jodie Anita McCutcheon, British Columbia Institute of Technology. Licensed under a Creative Commons Attribution 4.0 International License, except where otherwise noted. Download this book for free at http://open.bccampus.ca