Chapter 3 – Interprofessional Communication in Nursing
Conflicts in an Interprofessional Environment
Conflict can be defined as a state of serious opposition between two or more perspectives that influences thinking and actions. For example, people may disagree because they have different perspectives. However, varying perspectives alone do not lead to conflict: conflict emerges when one individual’s behaviours impede another individual’s interests or goals, resulting in negative emotions such as fear, anger, and frustration (Barki & Hartwick, 2004, as cited in RNAO, 2012).
Different perspectives will inevitably arise in any context, whether it is at work, with friends, or with colleagues. In an interprofessional environment, different perspectives will occur even when communication is relatively good. For example, healthcare professionals may have different disciplinary perspectives that inform their understanding of a situation, and may have different priorities in terms of client care. Communication can become problematic when these perspectives and priorities contradict another. Conflict is also more likely if interprofessional communication is sub-optimal and ineffective. Other factors that may contribute to conflict include lack of respect for others’ perspective, and differences in values, age, gender, education, ethnicity and culture, as well as elements related to professional roles such as responsibilities, power, and scope of practice (RNAO, 2012).
As shown in Figure 3.5, you can consider several strategies to prevent or manage conflict including:
- Use a client-centred approach to frame discussions.
- Use an evidence-informed approach to make decisions.
- Be open to hearing varying disciplinary perspectives.
- Engage in self-reflection.
- Engage in respectful discussions.
- Reflect on the perspectives of all team members.
- Share your perspective and rationale.
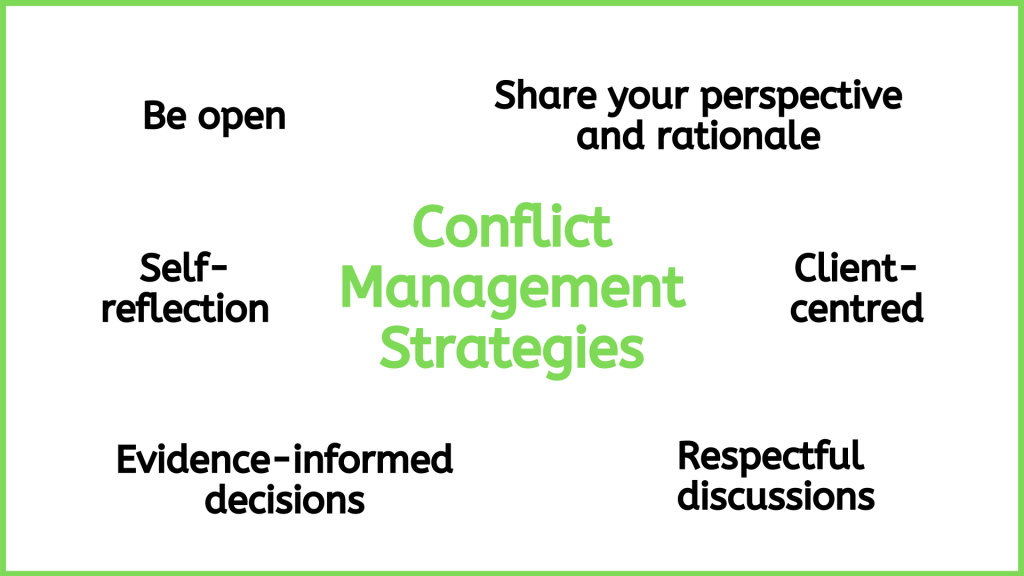
Figure 3.5: Conflict management strategies .
First, use a client-centred approach. This ensures the focus is on the client as a whole person and that the patient is cared for in ways that respect their “autonomy, voice, self-determination, and participation” in their own care (Registered Nurses Association of Ontario, 2006).
Second, use an evidence-informed approach. This will help you critically engage in discussions that are informed by the evidence, rather than personal preference. In addition, an evidence-informed approach can help to facilitate the professional growth of other members of the intraprofessional and interprofessional team by introducing them to new research and knowledge.
Third, it is essential that you be open to hearing, respectfully discussing, and reflecting on the perspectives of all team members (Lyndon et al., 2011). In addition to sharing your perspective, share the rationale for it. Along with a client-centred and evidence-informed approach, this kind of effective dialogue will benefit the person who is the focus of care and decisions: the client.
Points of Consideration
Interprofessional communication can be optimized using a client-centred perspective and an evidence-informed approach. It should be guided by discussions that are centred on the client’s wellbeing and incorporate the best possible evidence for each client.
Preventing and managing interprofessional conflict involves responsibility at both individual and systemic levels. The interpersonal nature of conflict is important, but contextual and organizational factors can also contribute. In the context of nursing, interprofessional team members are often working in environments where they are dealing with feelings such as frustration, burnout, dissatisfaction, and a sense of being undervalued. This kind of environment requires a high level of acuity and can be very emotionally draining.
It is imperative to consider whether healthcare organizations and systems are supporting collaboration and conflict resolution, or contributing to negative emotions (RNAO, 2012). For example, are processes and systems set up for easy communication? Do teams work together or are there divisions and hierarchies? Is there shared decision-making and accountability, or a culture of blame, disrespect, and fear of reprisal? Are certain health professionals particularly overworked? To prevent and reduce interprofessional conflict, the RNAO (2012) has developed specific recommendations for organizations to consider related to organizational structures and climate, leadership support, staffing practices, communication practices, and professional components.
The next section explores what can happen if conflicts are left unresolved and escalate to harassment and bullying.