Chapter 3 – Respiratory System Assessment
Anterior Thorax – Auscultation
Auscultating the anterior thorax involves the following steps (see Video 3.9):
1. Perform hand hygiene and cleanse the stethoscope.
2. Ensure the client is in an upright position and ask them to take a big breath in and out through the mouth each time they feel the stethoscope on their chest.
3. Place the stethoscope’s diaphragm on the chest in about three to six locations on each side of the anterior thorax so that you listen to all lung lobes. Ensure you have a complete seal. See Figure 3.16 for stethoscope placement pattern. Remember the number of locations depends on the size of the thorax; fewer locations are needed on a client with a smaller thorax (e.g., infants). Also remember that the anterior thorax has more upper lobes and that the right lung has three lobes while the left lung has two lobes.
- On the anterior thorax, begin at the lung apices, which are supraclavicular, moving from one side to the other side. As you move down the thorax, place your stethoscope close to the sternal line to avoid listening over the breast tissue. You may need to ask the client to reposition their breasts to place the stethoscope flat against the thorax. Toward the bottom, listen close to the sternal line and also move laterally.
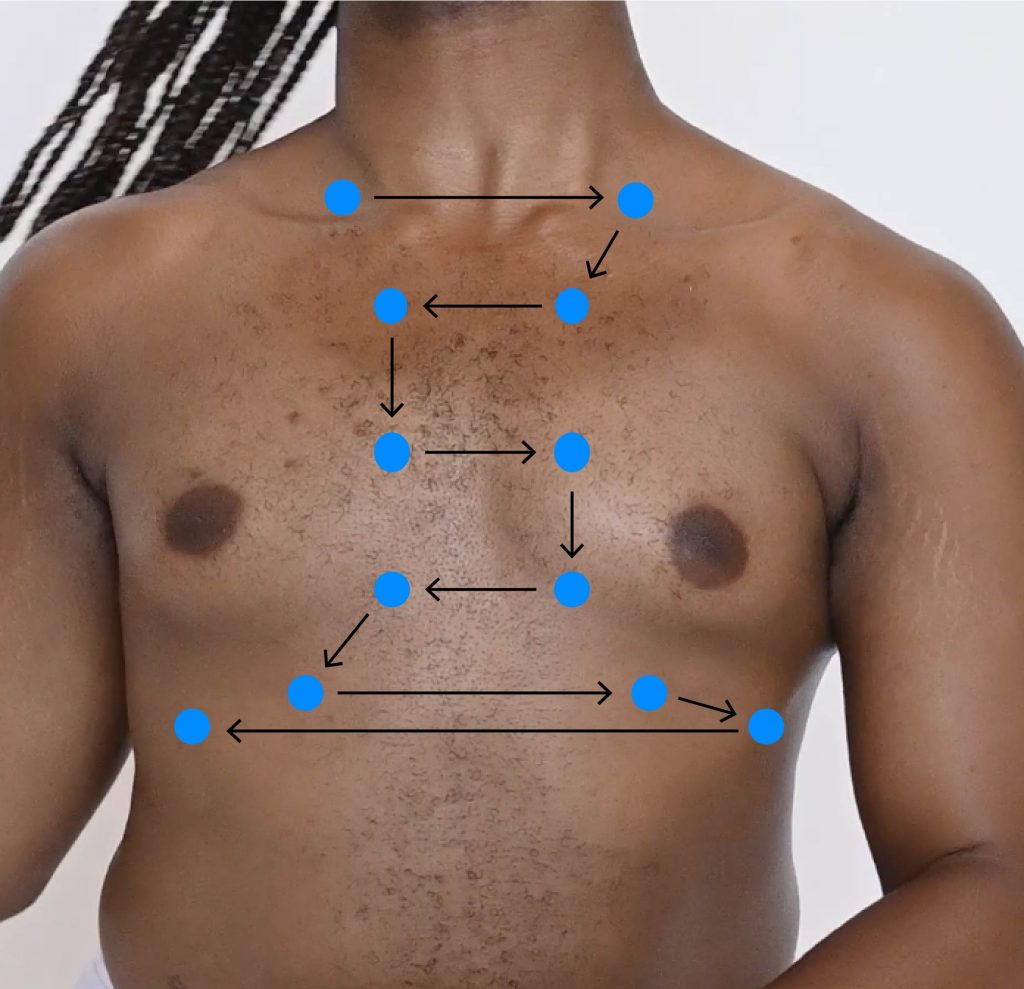
Figure 3.17: Stethoscope placement pattern when auscultating anterior thorax
Photo by Armin Rimoldi from Pexels (image was cropped and illustrated upon for the purposes of this chapter)
4. In each location, listen to one full respiration (inspiration and expiration) and compare air entry bilaterally.
5. Listen for the following:
- Air entry quality and equality.
- Quality: Note whether it is good, decreased, or absent.
- Equality: Note whether air entry is equal bilaterally.
- Identify the location of normal breath sounds including bronchial, bronchovesicular, and vesicular.
- If you place your stethoscope over the tracheal region, you should hear bronchial sounds (loud harsh sounds).
- Bronchovesicular breath sounds are moderate in loudness; inspiration is equal to the expiration phase, and heard on the upper thorax close to the sternum and near the bronchi.
- Vesicular breath sounds are quiet and low-pitched; inspiration is longer than the expiration phase, and heard in the periphery of the lung fields and near the smaller airways in an older child and adult. (Note: in young children particularly under two and threes of age, vesicular sounds are typically not heard because of their small thoraxes. Rather, you hear bronchovesicular).
- Identify clear air entry or the presence, quality, and location of any adventitious sounds.
6. Note the findings
- Normal findings might be documented as: “Good air entry, equal bilaterally, no adventitious sounds throughout all lobes on anterior thorax. Bronchovesicular sounds heard in upper lobes close to sternum. Vesicular sounds heard throughout peripheral lung field.”
- Abnormal findings might be documented as: “Absent air entry in right lower lobe anteriorly with mild wheezing heard upon expiration in the upper lobes bilaterally.”
Video 3.9: Auscultation of anterior thorax
Clinical Tips
For a client with breast tissue, you may need to have them reposition their breast so that you can place the stethoscope flat on their chest. This repositioning is also important when you palpate and percuss. It may feel awkward for the client to perform this action, so some nurses demonstrate on themselves over their own uniform to show the client what they would like them to do. Depending on where the breasts are positioned on the thorax, you may need to ask the client to reposition their breasts laterally and up or down. If the client is unable to do so, you may ask permission to reposition their breast. In this case, do so with the ulnar aspect of your hand. Avoid grasping or cupping the breast with your hand as this can be misinterpreted as a sexual motion. Always ask permission and inform the client what you will be doing in order to apply a trauma-informed approach and support the therapeutic nurse-client relationship.
Priorities of Care
The priorities of care related to auscultation of the anterior thorax are the same as those for the posterior thorax. Absence of air entry and presence of stridor are considered urgent situations: you should call for assistance and notify the physician or nurse practitioner. If you think the stridor is caused by a foreign body that you can quickly remove, do so. Otherwise, follow the steps of the primary survey (check airway patency, measure respiratory rate, work of breathing, and oxygen saturation, assess pulse rate/rhythm, blood pressure, assess level of consciousness). If the oxygen saturations are low, apply oxygen if you are permitted to do so. With the presence of crackles and wheezes, use the primary survey to determine whether there is a risk of clinical deterioration. Also consider whether the wheezing is new onset and could be caused by a severe allergic reaction (i.e., anaphylaxis) and requires immediate intervention. If not, and the client is stable, you can move the head of the bed up to assist with breathing and continue the focused assessment of the respiratory system.
Activity: Check Your Understanding