Chapter 4 – Cardiovascular System Assessment
Jugular Veins
Assessment of the jugular veins involves inspection of the pulsation. This assessment is performed because it provides information about the central venous pressure (CVP), which is the pressure in the vena cava near the right atrium and is an estimation of the right atrial pressure. Assessment of the CVP provides information about fluid status and functioning of the right ventricle.
When inspecting the jugular veins, you are noting whether there is elevated CVP as reflected by distention of the veins in the neck. Elevated CVP can be indicative of fluid retention, right ventricle contractile dysfunction that can be associated with heart failure, , , and tricuspid stenosis. Low CVP can be indicative of volume depletion (e.g., hemorrhage, dehydration).
You can assess CVP and other heart pressures with an invasive procedure called pulmonary artery catheterization. However, this would only be done in intensive care when the client is critically ill. A non-invasive way to assess the CVP is by inspecting the jugular veins
Inspection of Jugular Veins
1. Assist the client into a supine position with the head of bed in a position at least 30 degrees and no higher than 45 degrees. See Video 4.4.
- With normal CVP (not elevated), the jugular pulsation will not be visible if you raise the head of the bed to 90 degrees. With severely elevated CVP, you can raise the head of the bed to 90 degrees and still see the jugular pulsation.
2. Remove the client’s pillow so their head is laying flat against the bed in a neutral position. You may leave the pillow if it is flat (not fluffy). The important point is that the head, neck, and thorax are on the same plane and the neck is not flexed.
3. Stand on the right side of the bed and ask the client to gently turn their head to the left.
- It is assessed from the right side because the right jugular vein is more directly attached to the superior vena cava leading to the right atrium.
4. Use to highlight pulsations.
5. Begin by inspecting the right external jugular pulsation, as it is most visible. The vein should be flat or not visible; a bulging vein can suggest high CVP.
- The vein is superficial to the sternomastoid muscle and runs from anterior to the mastoid process to the medial portion of the clavicle. As it moves down to the clavicle, it becomes lateral to the sternomastoid muscle and then turns 90 degrees to join the superior vena cava. See Figure 4.3 as a reminder of the anatomy.
6. Next, inspect the right internal jugular pulsation at the sternal notch, the base of neck supraclavicular area, and up the neck as needed. The right internal jugular pulsation provides the most accurate assessment of the CVP because it attaches more directly to the superior vena cava. Note the location and the wave quality.
- A normal jugular pulsation is visualized around the sternal notch or the supraclavicular area. (The right internal jugular vein is underneath the sternomastoid muscle and runs from anterior to the mastoid process to the medial portion of the clavicle. It begins medial to the muscle at the mastoid process and then runs underneath the muscle as it moves down to the clavicle)
- The wave quality of a normal jugular pulsation is a double wave that is diffuse (diffuse means that it is spread out as opposed to in a pinpointed areas).
NOTE: Do not confuse the carotid artery pulsation with jugular venous pulsation. See Figure 4.3.
7. Note the findings
- Normal findings may be documented as: “Right external jugular vein is flat with no distension. Double diffuse pulsation of right internal jugular vein at sternal notch.”
- Abnormal findings may be documented as: “Bulging right external jugular vein. Accentuated double pulsation of right internal jugular vein just inferior to the ear lobe.”
Video 4.4: Inspection of the jugular pulsation
Clinical Tips
It is important to ensure your assessment is focused on the jugular pulsation and not the carotid pulsation. Unlike the carotid pulsation, the jugular pulsation varies with a person’s breathing, it is not palpable, and is not visible when the client is sitting upright unless they are experiencing severe distention. Additionally, the carotid pulsation is visualized as one quick wave in a specific area as opposed to a double diffuse wave.
Priorities of Care
A distended/bulging jugular vein (see Figure 4.4) is a critical finding in which blood is backing up from the right side of the heart/superior vena cava into the jugular veins; there are many causes such as , , and . It is typically associated with other cues such as heart palpitations, chest pain, tachycardia, perspiration, and dyspnea, and other signs of respiratory distress. The priority of care related to this cue is determining the cause and keeping the client stabilized. In addition to notifying the physician/nurse practitioner, you should continue monitoring the client’s vital signs (specifically: pulse, respiration, blood pressure, oxygen saturation) and continue the assessment with a focus on cardiac inspection, palpation, and auscultation. It is important to auscultate the valves to determine the quality of blood flow and presence of murmurs.
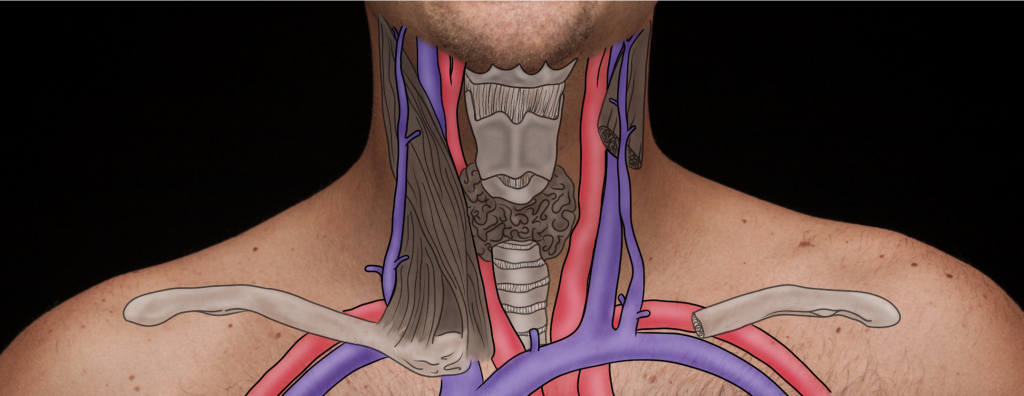
Figure 4.3: Jugular vein anatomy
Photo by engin akyurt on Unsplash (image was cropped and illustrated upon for the purposes of this chapter)

Figure 4.4: JVD by Ferencga is used under a Creative Commons Attribution-Share Alike 3.0 Unported license. (taken from: https://pressbooks.bccampus.ca/clinicalproceduresforsaferpatientcaretrubscn/chapter/2-8-head-to-toe-assessment-cardiovascular-assessment/)
Knowledge Bites – Pathophysiology
Jugular venous pulsation is influenced by blood volume, cardiac function of the right ventricle, and venous compliance. Any condition that causes an increase in right atrial pressure can lead to elevated CVP such as fluid overload, heart failure, pulmonary hypertension, and valve abnormalities (e.g., pulmonic stenosis).
Activity: Check Your Understanding
is inflammation of the pericardium, the layer of tissue surrounding the heart.
refers to high blood pressure in the pulmonary arteries.
refers to use of a penlight directed from the side as opposed to direct light at a 90 degree angle.
a condition that involves a weakening of the heart muscle affecting its ability to contract and pump out sufficient stroke volume.
refers to a narrowing of the tricuspid valve or when the valve does not close completely and bulges up into the atrium leading to regurgitation/leaking of blood backwards.