Chapter 2 – Inclusive Approaches to Health Assessment
What is an Inclusive Assessment?
To answer this question, let us first locate its relevance in the context of social justice.
Human existence is defined by differences: different people, experiences, cultures, and perspectives. Social justice is most commonly defined as fairness in terms of opportunities, regardless of differences.
Social injustice is rooted in differences and has led to terrible human suffering in our society. These injustices are the greatest point of weakness for humanity and come in many forms including:
- Racism (e.g., anti-Black, anti-Asian, anti-Indigenous racism)
- Inequality (e.g., sex, gender, racial inequality)
Social injustice can lead to social paralysis for some groups in society because of differential access to resources and opportunities, marginalization, exclusion, and discrimination. Social paralysis is a state of social stagnation imposed by inequity and injustice that hinders social and economic progress of groups in society.
Social injustice can also fuel what is known as “othering discourse” – discourse that promotes an “us” versus “them” mentality (Inokuchi & Nozaki, 2005). Othering is a process of exclusion and marginalization whereby groups of people are made to seem fundamentally different and inferior from dominant social groups, even to the point of making that group seem less than human. This can make marginalized groups feel unworthy and lead to powerlessness, fear, stress, trauma, and vulnerability to illnesses. From a health perspective, extreme manifestations of social injustice can include illnesses such as cancer, heart disease, diabetes, and respiratory disease. For example, researchers have demonstrated that structural injustices related to racism are the root cause of disparities in the prevalence and control of diabetes, as well as diabetes-related deaths, among racial and ethnic minorities (Ogunwole & Golden, 2021)
Without understanding the social roots of illness, it can be easy to blame clients for their illness outcomes, or even to perpetuate injustice in how a client is treated, with differential practices of health assessments across clients. All clients need to feel that their health and their health needs matter – and that they matter. Health assessments should make clients feel safe, respected, and engaged. If they feel marginalized or feel that they are being excluded or treated differently, this can foster injustices in their health outcomes, and in the healthcare system more broadly.
Inclusive health assessments should be grounded in social justice. Nurses must uphold the humanity of all clients in all aspects of care, regardless of the client’s race, ethnicity, gender, sexuality, age, ability, and any other factor that makes them who they are.
Inclusive health assessments are based on four key principles:
- Treat every health assessment as an act of humanity. What does it mean to be treated like a human being? We all want to be accepted, respected, and feel a sense of belonging. If you make a client feel otherwise, you are engaging in an act of oppression, which can affect human dignity and capacity to grow and transform. It is important to recognize that even though nursing is a caring profession, nurses have the to oppress. You must acknowledge differences among clients, while committing to dismantle social injustices within healthcare systems that render clients inhumane.
- Health assessments are not about sameness. Every client is different, so health assessments have to go beyond the “normal” or standardized approaches to physical assessment. “Normal” is a social construct: a common social idea based on cultural values and relative norms. You need to obtain a nuanced understanding of each client’s unique health and illness experiences and help them move towards a path of healing. A health assessment should be more than a physical assessment: talk with the client to obtain their health history and get to know them. An inclusive health assessment means that you recognize and integrate the client’s unique experiences and knowledge in their care.
- Examine your own personal biases. Everyone carries biases that are acquired through socialization. These may include biases about different races, cultural practices, body sizes, or religious practices. These biases can affect how you present yourself during a health assessment, and consequently how clients feel and respond in your presence. By learning about your own biases – how they developed and how they influence your actions – you can both understand how they lead to further injustices in nursing practice, and how you can start to unlearn them.
- Cultivate a safe environment of care. Create an environment where the focus is on what matters to the client. Approach each client with a “spirit of inquiry” (Registered Nurses’ Association of Ontario, 2007, p. 26). Keep an open mind as you learn about the client’s needs and perspectives: accept the client for who they are, value their feelings and experiences, and don’t judge them. A safe space is important for clients to express themselves without fear of being judged and discriminated against. Clients will engage more when they feel they are collaborating with the nurse on a common goal in terms of what is important to the client. Feeling safe promotes self-worth and a feeling of belonging, which are critical outcomes of social justice in the healthcare system.
Clinical Tip
Take a moment to test your own biases by taking the Harvard Implicit Association Test: https://implicit.harvard.edu/implicit/langchoice/canada.html When you go to this link, you can click on “Background” to learn more about the origins and purpose of this test or click on “Take a demo test” to test your biases.
The following diagram (Figure 2.1) shows how these key principles are inter-connected. You should incorporate all of them while engaging in an inclusive health assessment. As discussed above, social justice is central to inclusive health assessment, and is therefore located in the middle of the diagram. Importantly, as indicated, social justice is rooted in anti-oppressive perspectives, as discussed later in the chapter. The dotted line signifies the direct interaction between the practice of inclusive assessment in the healthcare system and its continuing impacts in communities.
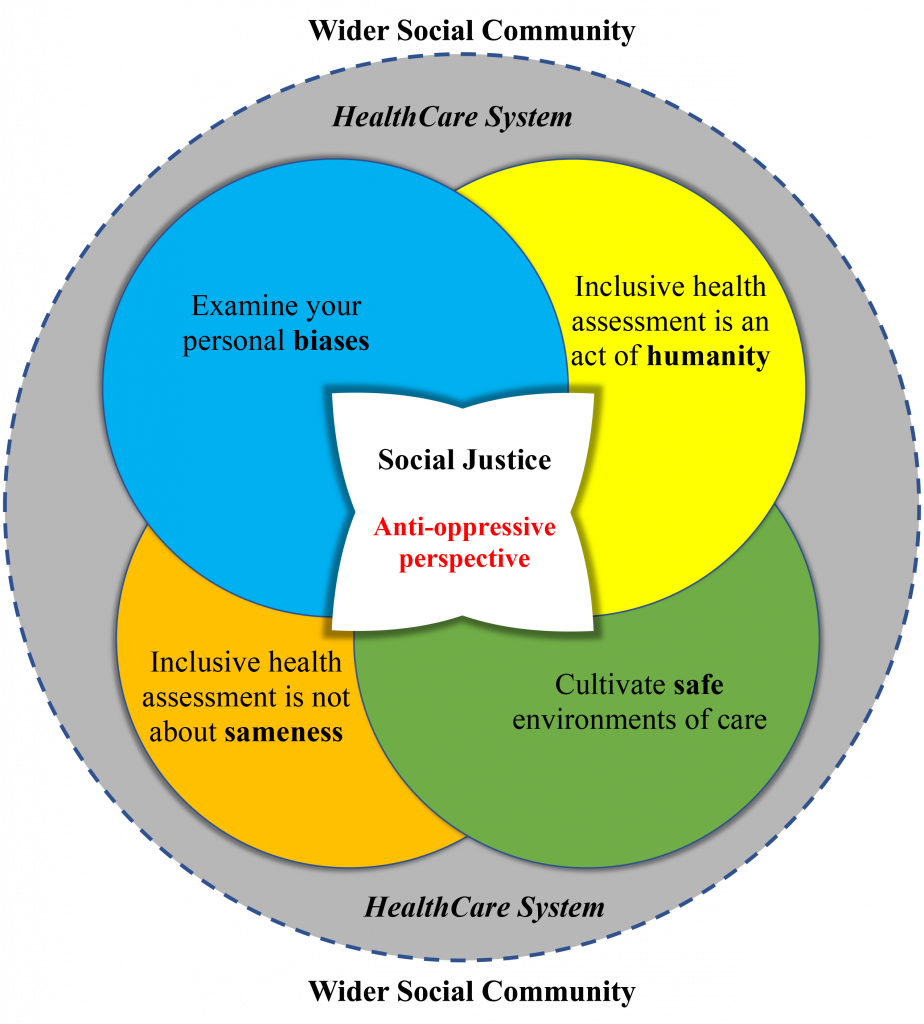
Figure 2.1: Principles of inclusive health assessments (illustrated by Levar Bailey)
Activity: Check Your Understanding
References
Inokuchi, H., & Nozaki, Y. (2005). “Different than Us”: Othering Orientalism, and US middle school students’ discourse on Japan. Asia Pacific Journal of Education, 25(1), 61-74. https://doi.org/10.1080/02188790500032533
Ogunwole, S. M., & Golden, S. H. (2021). Social determinants of health and structural inequities—root causes of diabetes disparities. Diabetes Care, 44(1), 11-13. https://doi.org/10.2337/dci20-0060
Registered Nurses’ Association of Ontario (2007). Healthy work environments best practice guidelines: Professionalism in nursing. Registered Nurses’ Association of Ontario. https://rnao.ca/sites/rnao-ca/files/Professionalism_in_Nursing.pdf
is prejudice and discrimination against individuals and groups based on age, usually older age.
is prejudice and discrimination against disabled people.
refers to the capacity to influence.