Chapter 4 – Cardiovascular System Assessment
Carotid Arteries
Assessment of the carotid arteries involves auscultation followed by palpation. This assessment provides information about cardiac function and the quality of blood flow through the artery.
Unobstructed blood flow is silent, whereas partial obstruction of blood flow (due to ) creates turbulent blood flow, leading to vascular sounds. These sounds are called bruits: blowing/swooshing noises. Following auscultation, if you do not hear bruits, proceed to palpating the carotid pulses. Be aware that complete obstruction of blood flow will also be silent, as there is no blood flowing through the artery.
This assessment is done in the seated position or in the high-fowlers position with the client looking straight ahead. Make sure they do not flex or extend their neck.
Auscultation of Carotid Arteries
1. Cleanse the stethoscope. See Video 4.2.
2. Ask the client to breathe in, breathe out, and then hold their breath.
- This is important because normal tracheal breath sounds can resemble a bruit and limit the nurse’s ability to hear the bruit. Note that some clients are unable to hold their breath for long: tell them to breathe if they feel they need to or if they become lightheaded.
3. With light pressure, place the stethoscope’s bell over the right carotid artery in the middle third of the neck, just medial to the sternomastoid muscle, but closer to the muscle than the trachea. This location is anatomically determined, see Figure 4.2.
- The bell should be used because vascular sounds are low-pitched.
- Usually, listening at one location on each side of the neck is sufficient. Some practitioners listen to three locations on the neck, but this is usually not needed because sound radiates. If you have concerns, you can listen to three locations on each side of the neck: at the base of the neck closer to the origin of the carotid artery; in the middle third of the neck just medial to the sternomastoid muscle, but closer to the muscle than the trachea; and inferior to the angle of the mandible.
4. Repeat the steps two and three on the left carotid artery.
5. Note the findings
- Normal findings might be documented as: “No carotid bruit present, bilaterally.”
- NOTE: You may hear the beating of the heart because sound travels.
- Abnormal findings might be documented as: “Carotid artery bruit present” (on left or right side or bilaterally).
Video 4.2: Auscultation of the carotid arteries
Priorities of Care
Do NOT palpate the carotid artery if you hear a bruit when auscultating the carotid arteries. A bruit can be a critical finding and is suggestive of carotid stenosis and partial obstruction of the artery. It is therefore important to not palpate (compress the artery) when the blood flow is already compromised. You should measure the client’s vital signs (specifically pulse, blood pressure, oxygen saturation, respiration) and continue the cardiac assessment. Then, report your findings to the physician/nurse practitioner.
Palpation of Carotid Arteries
1. First, if you hear a bruit when auscultating the carotid arteries, do not palpate the carotid artery. Only proceed with palpation if you do not hear a bruit. See Video 4.3.
2. Place the pads of your three fingers gently over ONE carotid artery (right or left) in the middle third of the neck, just medial to the sternomastoid muscle. Then, repeat on the opposite artery.
- Do NOT palpate the left and right carotid arteries at the same time, because this can compromise blood flow superior to the location you are palpating (the brain).
- Do NOT place the pads of your finger high on the neck, because this area is the location of the baroreceptors of the carotid sinus. These receptors are medial to the sternomastoid muscle, inferior to the angle of the jaw, and just superior to the thyroid cartilage. They play a role in mediating heart rate and blood pressure, and increased pressure on this area can lead to bradycardia and a drop in blood pressure.
3. Palpate for the following:
- Force (strength of pulsation). Pulse force is recorded using a four-point scale:
-
- 3+ Full, bounding
- 2+ Normal/strong
- 1+ Weak, diminished, thready
- 0 Absent/non-palpable
(Adapted from: Vital Sign Measurement Across the Lifespan, 2nd Canadian edition)
- Symmetry (compare force between left and right side).
- Quality (describe the pulsation) in terms of the wave form. The carotid pulsation is described as a quick upstroke (one cursory/brisk outward movement felt against your fingers) and a slow downstroke (a more gradual inward movement away from your fingers).
4. Note the findings
- Normal findings may be documented as: “2+ carotid pulsation equal bilaterally, smooth contour with a quick upstroke and gradual downstroke.”
- Abnormal findings may be documented as (example): “1+ carotid pulsation bilateral with and gradual downstroke” (reduced amplitudes can be common in conditions with low stroke volume, while dicrotic upstrokes can be common with increased peripheral vascular resistance, for example in situations of heart failure).
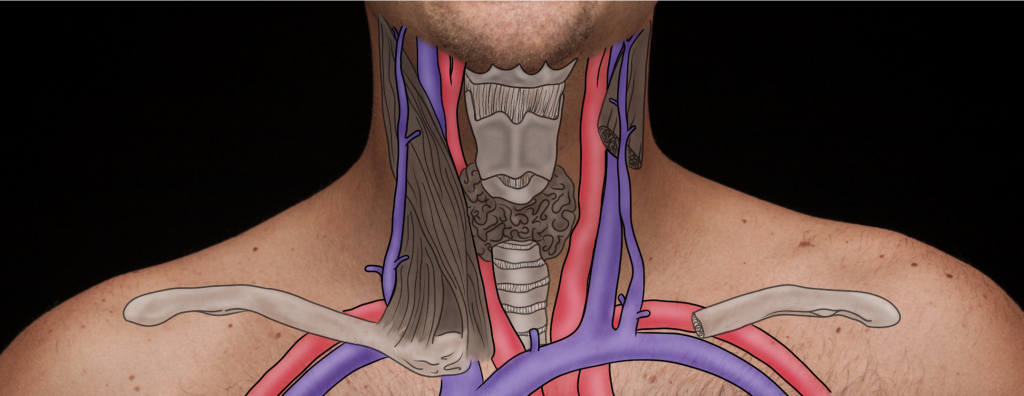
Figure 4.2: Carotid artery anatomy
Photo by engin akyurt on Unsplash (image was cropped and illustrated upon for the purposes of this chapter)
Video 4.3: Palpation of carotid arteries
Activity: Check Your Understanding
is the narrowing of the carotid artery.
is an abnormal double beat of the carotid artery.