Lymphatic System Assessment
Assessment of Lymphedema
Assessment of the lymphatic system includes inspecting the skin for signs of lymphedema (Figure 5 shows signs of severe edema). The most common sign is swelling, but other signs may be present when the condition is severe or not well managed.


Figure 5: Lymphedema.
(Attribution: Photo of legs by Medical doctors – https://commons.wikimedia.org/w/index.php?curid=37663127 and photo of arms has been cropped. Photo by DocHealer – https://commons.wikimedia.org/w/index.php?curid=64120555, both own work, CC-BY SA 4.0)
Clients with lymphedema will usually report that they are experiencing swelling or that their clothes or jewelry appear to be fitting tighter. This will help you to determine where to begin your assessment. If you are doing a general assessment, it is appropriate to observe the face, neck, arms and legs in a sitting or supine position. Observe the client’s bare skin and compare bilaterally.
Assessment for lymphedema involves the following steps:
- Inspect for swelling and symmetry over the face, neck, arms, and legs.
- Normally, no swelling is present on the face, neck, arms, and legs, and limb circumference is equal bilaterally.
- If swelling or asymmetry is present, describe the location. If you observe asymmetrical limbs in terms of circumference, measure with a flat/flexible tape measure around the largest area of swelling on the affected limb and measure at the same location on the other limb.
If you note swelling, assess for pitting edema: an indentation that remains after applying pressure over the location (see Figure 6). Apply pressure with the pad of your finger on a distal location (feet and medial malleolus) for about 3-5 seconds and then release. If you observe an indentation (a “pit”), note the location and how long the indentation remains. Then, assess a proximal location to assess how high the edema goes (e.g., over the tibia). Always check with the unit you work on about the scale used to evaluate pitting edema. Scales are usually 1–4 as shown in Figure 7 and are used to record the pit depth and rebound time (the time for the indentation to disappear). Often, 1 is classified as mild, 2 as moderate, 3 as severe, and 4 as very severe.

Figure 6: Example of pitting edema
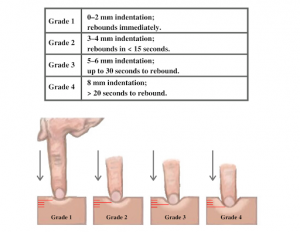
Figure 7: Pitting edema scale. (Attribution: https://wtcs.pressbooks.pub/nursingskills/ CC-BY 4.0).
- Inspect for skin discolouration, skin breakdown (cuts, cracks), and ulcers over the face, neck, arms, and legs. Inspect anterior and posterior sides, in between skin folds and toes, and on the bottom of the feet.
- Normally, skin colour is even throughout the body and skin is intact.
- If you observe any skin discoloration from the client’s baseline, identify the location and colour. If skin is not intact or ulcers are present, note the location and record a description. If applicable, describe the colour, odour, and colour and quantity of discharge.
- Palpate for temperature using the dorsa of your hands from the top of the client’s limb (e.g., shoulder/upper leg) to their extremities (hand/fingers and feet/toes).
- Normally, the temperature is equal bilaterally. The distal portions of the limbs (hands and feet) may be slightly cooler, but should be equal bilaterally.
- If you note any asymmetry in temperature or extreme temperatures, identify the location and temperature (i.e., cold or hot).
- Palpate skin texture and consistency with your first two or three fingers and thumb over the limbs or any areas where lymphedema is suspected.
- Normally, the skin texture is smooth and soft with no lumps.
- Describe the quality and note the location of any dry, moist, dimpled, or firm areas on the skin.
- If you suspect lymphedema, assess the client’s mobility of the affected limb and range of motion.
- Normally, clients should have no difficulty moving their arms and legs, with full range of motion and no pain.
- Note any difficulty moving, limited range of motion, or pain.
- Note the findings:
- Normal findings might be documented as: “No swelling or discolouration present on the face, neck, arms, and legs, and limb circumference is equal bilaterally. Temperature is warm to touch and equal bilaterally, and skin texture is smooth with no lumps on arms and legs.”
- Abnormal findings might be documented as: “Redness and swelling noted on left arm, left upper arm circumference 19 inches and forearm circumference 12 inches. Right upper arm circumference 14 inches and forearm circumference 10 in inches. Full range of motion of both arms. Client describes slowness and difficulty moving arm.”
Priorities of Care
A main priority of care is to prevent and/or treat infection. Clients with lymphedema are at risk for skin breakdown, ulcers, and infection. Skin should be kept clean, dry, and moisturized. Clients should also be careful to prevent any scratches or cuts that could lead to infection. Assess and monitor any areas of the skin that are not intact and/or show potential infection. It is important to observe if any areas of concern worsen (e.g., get bigger). Report to the physician or nurse practitioner if you observe any ulcers or signs of infection.
Clients with lymphedema may be referred to a physiotherapist and encouraged to perform light exercises to assist with lymphatic fluid transportation. For similar reasons, compression stockings are often prescribed: these are fitted elastic stockings that apply a certain amount of pressure to the limb. It is also often recommended to elevate limbs with lymphedema.
Activity: Check Your Understanding
refers to the degree of density or firmness.