Pain Assessment
Classifying Pain
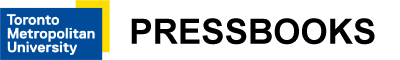
Pain can be classified in many ways. The next sections present several classifications. It is important to recognize that these are not mutually exclusive, and a person may experience multiple classifications of pain at the same time. See Figure 1 for classifications of pain.
Figure 1: Classifications of pain.
Acute Pain
Acute pain is short or limited in duration and often caused by something specific. Types of acute pain are surgical pain during the operative and postoperative period, a headache, bee sting, labour pains, menstrual pain, and injuries such as an ankle sprain, fracture, or burn. Although acute pain can shift into chronic pain, it typically follows a predictable trajectory and subsides when the cause of pain is resolved or healed. Acute pain can last anywhere from a moment to upwards of three to six months. Beyond this timeframe, it is typically considered chronic pain.
The intensity of acute pain can range from mild to severe. The intensity may also influence the signs and symptoms of pain that are associated with sympathetic nervous stimulation and the fight or flight response including the stimulation of hormones such as cortisol and adrenaline.
The cascade of signs and symptoms during the acute pain period may include:
- Changes in vital signs: tachycardia, tachypnea, shallow breathing, elevated blood pressure, and elevated temperature. Sometimes oxygen saturations can decrease, particularly when clients are breathing fast and shallow and as such not taking a full inspiration. Prolonged changes in these vital signs can lead to ischemia, thus pain management is essential.
- With increased body temperature, the nervous system stimulates the sweat glands to help cool the body. Thus, clients may experience diaphoresis.
- Digestive enzymes and peristalsis are reduced which leads to difficulty with digestion and gastrointestinal upset including nausea, vomiting, and constipation.
- Other signs of pain may include increased blood glucose levels and pupil dilation.
Chronic Pain
Definitions of chronic pain have evolved and become more specific, but this kind of pain is still referred to as pain that continues to occur and recurs (persistent and recurrent) for about three months or more (Treede et al., 2019). Some definitions suggest six months or more, but in general it is fine to refer to persistent or recurrent pain that lasts three to six months or longer as chronic pain. Another conceptualization of chronic pain (when associated with an injury) is a type of pain that persists beyond the typical or expected healing time. For some, chronic pain never goes away: it may be experienced daily or recur regularly.
Common types of chronic pain include back pain, migraines, arthritis, cancer-related pain, , and postsurgical and posttraumatic pain.
Chronic pain can be categorized in two broad ways:
- Secondary chronic pain refers to a type of pain that manifests as a result of a disease or condition such as arthritis, cancer, or ear infection – it is “secondary” to these pathological conditions (Treede et al., 2019). It can also be pain that is secondary to, or a result of, treatment such as cancer-related treatment.
- Primary chronic pain is a more recent classification. It is a type of pain based on a condition that is often poorly understood and cannot be accounted for by another cause or disease process (Nicholas et al., 2019; Treede et al., 2019, 2015). Common types of primary chronic pain include many types of neck and back pain, fibromyalgia syndrome, and irritable bowel syndrome (Nicholas et al., 2019).
In patients with chronic pain, the physiological and vital sign changes are not necessarily evident because the body adapts to the pain to a certain extent. The effects of chronic pain typically include cognitive and social changes, such as:
- Sleep disruptions.
- Mood disturbances including depression.
- Interference with daily activities.
- Cognitive impairment including the ability to think clearly.
- Social and relational effects.
Nociceptive Pain
Nociceptive pain involves a noxious stimulus (mechanical, thermal, or chemical) that activates nociceptors with the potential to cause non-neural tissue injury (Bonezzi et al., 2020). This is a common type of pain that many of us have experienced and is often categorized as:
- Mechanical (e.g., stubbing your toe, receiving a needle, straining a muscle).
- Thermal (e.g., touching a hot surface like a stove).
- Chemical (e.g., exposure to a chemical such as bleach).
(Bonezzi et al., 2020).
These stimuli activate the nociceptors, which are receptors in the periphery of the (IASP, 2021). Considering these stimuli, it makes sense that nociceptive pain is described as localized with a specific location in the body. Nociceptive pain can be categorized as somatic and visceral. Somatic refers to a type of pain that originates in peripheral tissues such as the skin, bone, muscles, tendons, or ligaments, whereas visceral refers to a type of pain that originates in the body’s internal organs (e.g., heart, intestines, appendix, kidneys) (Bonezzi et al., 2020).
Neuropathic Pain
Neuropathic pain originates from a “lesion or disease of the somatosensory nervous system” (IASP, 2021). Neuropathic pain has a different subjective sensation than nociceptive pain and is often described as burning, stabbing, numbness, tingling, and shooting (electric-shock like) with sensitivity to touch and temperature. As such, the client’s qualitative description of their pain is important to assess in order to help you better understand the causative factors. Causes can be related to trauma along a nerve, conditions such as carpal tunnel syndrome, spinal cord injury, stroke, diabetes, and multiple sclerosis, and infections such as herpes simplex virus (cold sore) or varicella-zoster virus (shingles).
Nociplastic Pain
Nociplastic pain originates from “altered nociception” with unclear evidence of actual or potential tissue damage (IASP, 2021). This classification of pain has no obvious nociceptor activation or neuropathy, but involves altered nociceptive function, which can be confirmed by sensory testing (Kosek et al., 2016). To be clear: although there is no obvious tissue damage (e.g., a cut in the skin) or nociceptor activation (a stimulus that has caused pressure or extreme temperature to activate the neurons), there is an inference of altered nociceptive function that can be confirmed through sensory testing such as measuring the brain’s electrical activity (Kosek et al., 2016). This classification is relatively new compared to nociceptive and neuropathic pain and was introduced in 2016 (Kosek et al., 2016). The theory is that nociplastic pain is associated with chronic pain conditions such as fibromyalgia and irritable bowel syndrome (Kosek et al., 2016; Bonezzi et al., 2020). It requires careful consideration in terms of assessment and management because of the complexity in how it presents subjectively as well as the lack of (Fitzcharles et al., 2021).
Idiopathic Pain
Idiopathic pain or pain of an unknown origin can also be considered a fourth classification. With this type of pain there is no obvious pathology. Although the origin and the cause may be unknown, the pain is very real for clients. Your assessment here becomes extremely important to help understand the client’s pain.
Referred Pain
Referred pain is pain felt at a bodily location that is different from the site of origin. For example, the site of origin of cardiac ischemia (lack of oxygen to the heart muscle, commonly referred to as chest pain) is the heart. However, cardiac ischemia can be felt in referred locations such as pain down the left arm or in the jaw or neck. This kind of pain referral has a neural basis in which the site of origin shares common neural pathways with another part of the body. See Figure 2 for common pain referral pathways.
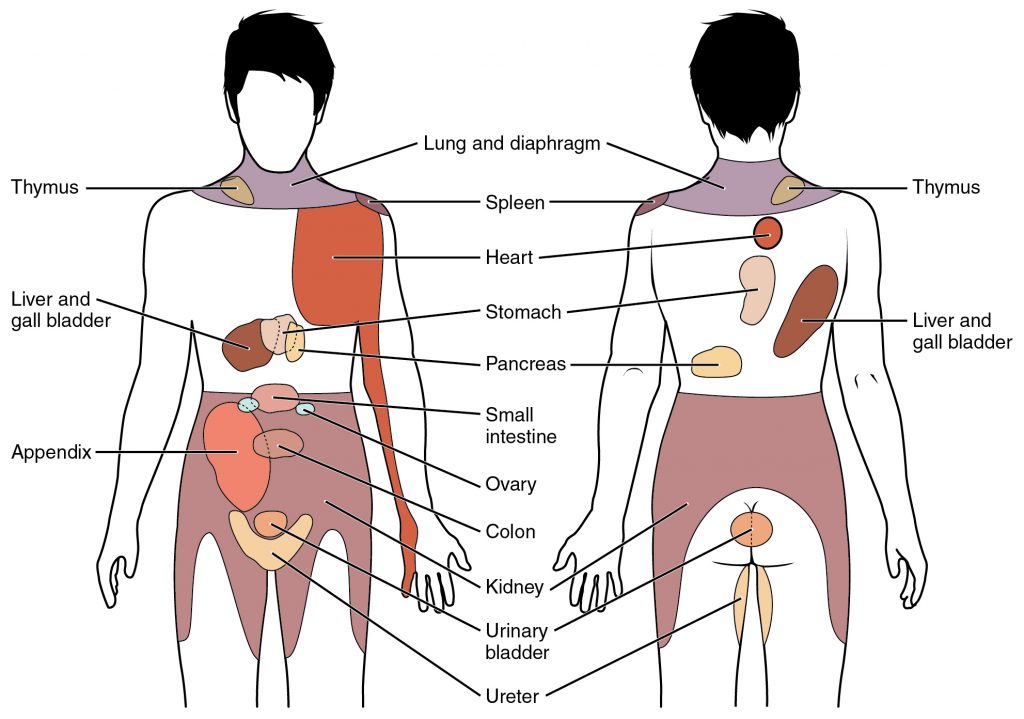
Figure 2: Common pain referral pathways
Attribution statement: Gordon Betts, J., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., & DeSaix, P. (2013). The Autonomic Nervous System. In Anatomy and Physiology. OpenStax. Creative Commons Attribution License v4.0. Book URL: https://openstax.org/books/anatomy-and-physiology/pages/1-introduction Section URL: https://openstax.org/books/anatomy-and-physiology/pages/15-2-autonomic-reflexes-and-homeostasis
Activity: Check Your Understanding
References
Bonezzi, C., Fornasari, D., Cricelli, C., Magni, A., & Ventriglia, G. (2020). Not all pain is created equal: Basic definitions and diagnostic work-up. Pain and Therapy, 9(Suppl 1), 1-15. https://doi.org/10.1007/s40122-020-00217-w
Fitzcharles, M., Cohen, S., Clauw, D., Littlejohn, G., Usui, C., & Häuser, W. (2021). Nociplastic pain: Towards an understanding of prevalent pain conditions. The Lancet, 397(10289), 2098-2110. https://doi.org/10.1016/S0140-6736(21)00392-5
International Association for the Study of Pain (2020). IASP announces revised definition of pain. https://www.iasp-pain.org/publications/iasp-news/iasp-announces-revised-definition-of-pain/
International Association for the Study of Pain (2021). Terminology. https://www.iasp-pain.org/resources/terminology/#pain
Kosek, E., Cohen, M., Baron, R., Gebhart, G., Mico, J., Rice, A., Rief, W., & Sluka, K. (2016). Do we need a third mechanistic descriptor for chronic pain states? Pain: The Journal of the International Association for the Study of Pain, 157(7), 1382-1386. https://doi.org/10.1097/j.pain.0000000000000507
Nicholas, M., Vlaeyen, J., Rief, W., Barke, A., Aziz, Q., Benoliel, R., Cohen, M., Evers, S., Giamberardino, M., Göbel, A., Korwisi, B., Perrot, S., Svensson, P., Wang, S., & Treede, R. (2019). The IASP Taskforce for the Classification of Chronic pain. The IASP classification of chronic pain for ICD-11: chronic primary pain. Pain: The Journal of the International Association for the Study of Pain, 160(1), 28–37. https://doi.org/10.1097/j.pain.0000000000001390
Treede, R., Rief, W., Barke, A., Azia, Q., Bennett, M., Benoliel, R., Cohen, M., Evers, S., Finnerup, N., First, M., Giamberardino, M., Kaasa, S., Korwisi, B., Kosek, E., Lavand’homme, P., Nicholas, M., Perrot, S., Scholz, J., Schug, S., Smith, B., Svensson, P., Vlaeyen, J., & Wang, S. (2019). Chronic pain as a symptom or a disease: The IASP Classification of Chronic Pain for the International Classification of Disease (IDC-11). Pain: The Journal of the International Association for the Study of Pain, 160(1), 19-27. https://doi.org/10.1097/j.pain.0000000000001384
Treede, R., Rief, W., Barke, A., Aziz, Q., Bennett, M., Benoliel, R., Cohen, M., Evers, S., Finnerup, N., First, M., Giamberardino, M., Kaasa, S., Kosek, E., Lavand’homme, P., Nicholas, M., Perrot, S., Scholz, J., Schung, S., Smith, B., Svensson, P., Vlaeyen, J., & Wang, S. (2015). A classification of chronic pain for ICD-11. Pain: The Journal of the International Association for the Study of Pain, 156(6), 1003-1007. https://doi.org/10.1097/j.pain.0000000000000160
is a chronic condition that causes pain and discomfort all over the body as well as fatigue.
refers to the network of nerve cells throughout the brain and body that produce the perception pain and other sensations such as touch and temperature.
refer to objective characteristics that can be measured as an indicator of a condition or disease. These can be molecular, histologic, radiographic, or physiological characteristics such as blood tests, x-rays, and vital signs.