Enteral Nutrition
Plan
Page Contents
Team Rounds

Common PES Statement Terminology
As you interpret the data from the assessment, you can form PES statements or nutrition diagnoses that help identify nutrition concerns that need to be addressed in your plan. If you are not familiar with how to write a PES statement please review this resource from the Academy of Nutrition and Dietetics. Here are some common nutrition problems that patients requiring enteral nutrition may have:
- Inadequate energy intake
- Inadequate protein intake
- Inadequate oral intake
- Inadequate fluid intake
- Increased nutrient needs
- Malnutrition
- Inadequate vitamin/mineral intake
- Swallowing difficulty
- Impaired GI function
- Intake of unsafe food
- Physical inactivity
- Inability or lack of desire to manage self-care
Carson’s PES Statements
Based on our assessment here are some sample PES statements for Carson. Pause and practice writing other PES statements for Carson!
- Inadequate protein-energy intake related to esophageal cancer and 6-month history of progressive dysphagia as evidenced by dietary recall (low protein and energy intake), loss of appetite and 25 lbs weight loss.
- Inadequate oral intake related to 6-month history of progressive dysphagia as evidenced by loss of appetite, dietary history (consumption of ~500 kcal/day) and 25 lbs weight loss.
- Malnutrition related to a 6-month history of esophageal cancer resulting in progressive dysphagia as evidenced by low serum lab values (potassium, phosphorus, ), poor oral intake, dietary history (consumption of ~500 kcal/day), physical assessment and 25 lbs weight loss.
Enteral Nutrition Planning
Below are the steps for creating a comprehensive enteral nutrition feeding plan.
- Summarize and utilize assessment data (energy, protein, fluid requirements).
- Determine enteral formula (hospital specific formulary) and calculate goal feeding volume/ rate.
- Conduct refeeding syndrome assessment (to adjust starting rate/ advancement of feeds if appropriate)
- If no risk of refeeding syndrome determine administration schedule, starting rate & rate of advancement (volume/time).
- Based on goal feeding rate, calculate the following:
- Energy (kcal/day) & (kcal/kg), protein (g/day) & (g/kg), free water (mL/day) & (mL/kg), fibre (g/day), % DRI of relevant vitamins and minerals.
- If patient is at risk of refeeding syndrome calculate amount of CHO when initiating feeds (g/day) and at goal rate (g/day).
- Calculate the required amount of free water flushes for tube and/or hydration (consider all sources of fluid — IV and medications as well as fluid restrictions).
- Consider adding a multivitamin and/or other supplements (i.e. Vitamin D).
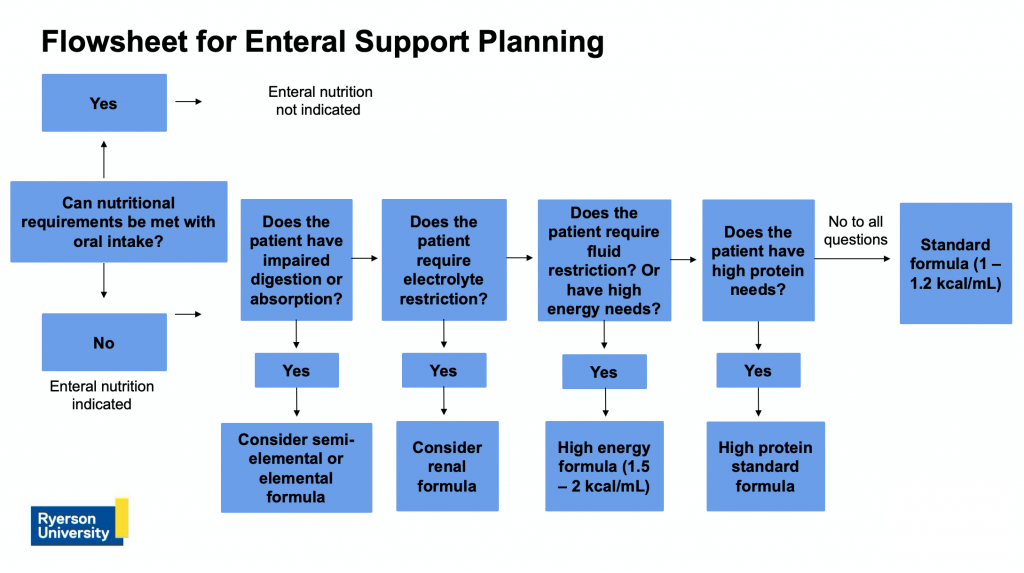
Flowsheet
A flowsheet to support enteral planning is presented below. When selecting a plan and formula, it is important to ask yourself the questions listed in the flowsheet. These questions are not comprehensive and you may ask additional questions or encounter other considerations that impact formula section. However, this is a good starting point.
Practice Formula Sheet
Refer to the tables below for a practice formula sheet, broken down into three parts: tube feeds, nutrient modules, and meal supplements.
Depending on your hospital’s formulary, you may have other options to select from. However, this sheet gives you all the information you need to select a formula and determine the nutritional content for your patients needs. You can use this sheet to practice additional calculations outside of our case study. If you are using a pre-made sheet or create your own formulary, always check the supplier’s website to confirm it is up to date as products change over time.
| TUBE FEED | Kcal/mL | Protein (g/mL) |
Fat (g/mL) |
CHO (g/mL) |
Fibre (g/mL) | %H20 | Na (mg) |
K (mg/mmol) |
Cl (mg) |
Fe (mg) |
P (mg) |
Ca (mg) |
Mg (mg) |
Zn (mg) |
mOsm /kg H2O |
Volume to meet DRI | Features/Indications (all low lactose, gluten free) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Isosource Fibre 1.2 | 1.2 | 0.054 | 0.04 | 0.16 | 0.015 | 80 | 1.1 | 1.9/0.049 | 1.3 | .014 | 0.96 | 0.96 | 0.34 | 0.016 | 480 | 1250 ml | Fibre (pea, OS, inulin acacia) 0.015 g/ml |
| Isosource 1.5 | 1.5 | 0.068 | 0.06 | 0.17 | 0 | 76 | 1.3 | 2.4/0.06 | 1.6 | 0.018 | 1.2 | 1.2 | 0.42 | 0.02 | 530 | 1000 ml | Energy dense, moderate protein |
| Isosource 1.0 HP | 1 | 0.064 | 0.034 | 0.11 | 0 | 83 | 0.88 | 1.6/0.041 | 0.9 | 0.014 | 0.8 | 0.8 | 0.28 | 0.016 | 330 | 1500 ml | High protein, no fibre |
| Novasource Renal | 2 | 0.091 | 0.1 | 0.19 | 0 | 72 | 0.95 | 0.95/0.024 | 0.8 | 0.018 | 0.835 | 0.84 | 0.2 | 0.022 | 800 | 1000 ml | For renal failure, electrolyte & fluid restriction. |
| Peptamen Intense 1.0 High Protein | 1 | 0.092 | 0.038 | 0.076 | 0.004 | 84 | 0.68 | 1.36/0.036 | 1.12 | 0.012 | 0.68 | 0.68 | 0.28 | 0.024 | 345 | 1500 mL | Very high protein, semi elemental, prebiotic, fish oil |
| NUTRIENT MODULE | Kcal/mL | Protein (g/mL) |
Fat (g/mL) |
CHO (g/mL) |
%H20 | Na (mg) |
K (mg/mmol) |
Cl (mg) |
Fe (mg) |
P (mg) |
Ca (mg) |
Mg (mg) |
Zn (mg) |
mOsm /kg H2O |
Volume to meet DRI | Features/Indications (all low lactose, gluten free) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Beneprotein (per 7g pkg) |
25 | 6 | 0 | 0 | 0 | 15 | 35/0.9 | – | – | – | – | – | – | – | – | Protein supplement 1 scoop = 1 package = 7 g = 21 ml powder |
| MEAL SUPPLEMENT |
Kcal/mL | Protein (g/mL) |
Fat (g/mL) |
CHO (g/mL) |
Fibre (g/mL) | %H20 | Na (mg) |
K (mg/mmol) |
Cl (mg) |
Fe (mg) |
P (mg) |
Ca (mg) |
Mg (mg) |
Zn (mg) |
mOsm /kg H2O |
Volume to meet DRI | Features/Indications (all low lactose, gluten free) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ensure Regular | 1.06 | 0.04 | 0.029 | 0.15 | 0 | 84 | 0.45 | 0.68/0.017 | 0.45 | 0.016 | 1.6 | 1.28 | 0.28 | 0.017 | 642 | – | Low residue |
| Ensure Plus | 1.5 | 0.06 | 0.047 | 0.22 | 0 | 77 | 0.45 | 0.72/0.018 | 0.45 | 0.016 | 1.17 | 1.28 | 0.28 | 0.017 | 633 | – | Energy dense |
Carson’s Enteral Regime
- Current weight: 59 kg
- Carson’s nutrition requirements:
- Energy: 1770-1800 kcal/day (~30 kcal/kg/day)
- Protein: 71-77 g/day (1.2-1.3 g/kg/day)
- Fluid: 2065 mL/day (35 mL/kg/day)
- Formula selection: Isosource 1.2 (standard formula)
- Continuous feeding: over 20 hours
- It is common to start enteral nutrition on a patient like Carson with a continuous feeding schedule. He has had a prolonged period of low intake and he is at risk of refeeding syndrome. A continuous feeding schedule will allow us to assess GI and metabolic tolerance.
- We are feeding over 20 hours because there is a drug-nutrient interaction with levothyroxine, so we need to hold feeds 2 hours before and after administration. Check your institution’s policy about holding feeds for drug-nutrient interactions.
Review the requirements and practice calculating Carson’s enteral feeding plan using the formulary sheet provided.
Calculations:
- Formula amount: 1800 kcal ÷ 1.2 kcal/mL = 1500 mL/day (at goal volume the DRIs are met)
- Goal rate: 1500 mL ÷ 20 hours = 75 mL/hr
- Provides:
- Energy: 1.2 kcal/mL × 1500 mL/day = 1800 kcal/day (30 kcal/kg)
- Protein: 0.054 g/mL × 1500 mL= 81 g/day (1.3 g/kg)
- Carbohydrate: 0.16 g/mL × 1500 mL = 240 g/day
- Fat: 0.04 g/mL × 1500 mL = 60 g/day
- Free water: 80% of 1500 mL = 1200 mL/day
- For this amount of formula, there is 1200 mL of free water, which does not meet his estimated requirements for fluid. This is important to keep in mind when calculating water flushes and evaluating other sources of fluid.
Carson’s Enteral Regime: Water Flushes
Prior to calculating Carson’s water flushes, liaise with his MD/ to change his IVF to 0.9% NS and decrease his rate to 10 mL/hr. Carson will be receiving ~1200 mL free water from his enteral feeds (at goal rate) and will have a continuous source of CHO (does not require ⅔ + ⅓). Patients typically receive 10-25 mL/hr TKVO (to keep vein open).
He is also receiving ~300mL of water for his medication administration. This is information you obtained from his nurse.
Calculate water flushes required for a total fluid intake (TFI) of ~2065 mL/day (35 mL/kg)
- Current sources:
- IV 0.9% NS @ 10 mL/hr = 240 mL/day.
- ~1200 mL free water from his enteral feeds (at goal rate)
- ~300 mL from medication administration
- Current total fluid delivery: IV (240 mL) + medications (300 mL) + feeds (1200 mL) = 1740 mL/day (29 mL/kg)
- Fluid deficit = 2065 mL − 1740 mL = 325 mL/day needed via flushes
- 325 mL ÷ 50 mL flushes (for tube patency) = ~6 times per day
- TFI to meet needs: 240 (IV) + 300 (meds) + 1200 (feeds) + 50×6 (water flushes) = 2040 mL/day (35 mL/kg)
- Order water flushes: 50 mL via G-Tube q 4 hours
It is common practice to flush the feeding tube for patency every 4-6 hours with a minimum of 25 mL of water. For Carson, we will order 50 mL water flushes q 4 hrs to meet his needs of approximately 35 mL/kg of fluid per day.
Protocol for Starting Enteral Nutrition
When starting enteral nutrition, the general protocol is to:
- Start continuous feeding at a slow rate to evaluate tolerance (10-40 mL/hr). If tolerated, increase by increments of 10-25 mL every 4-12 hrs to reach goal rate.
- Consider the hang time of formula: maximum 8 hours per carton to prevent bacterial contamination. If the hourly rate is low, pour half the carton into the enteral feeding bag and discard the remainder
- Flush the feeding tube with water (25-50 mL) every 6 hours for tube patency (minimum – may need increased water flushes depending on formula, tube size, or medications ordered).
- Always evaluate refeeding risk and follow the appropriate implementation practices, if warranted
When your patient is at risk of refeeding syndrome, you should:
- Initiate feeding as soon as possible.
- Eetermine caloric and protein requirements using current weight
- Start nutrition slowly via continuous infusion
- Energy: no more than 50% of energy requirements in the first 24 hrs, maximum 15-20 kcal/kg (if at severe risk: ≤10 kcal/kg).
- Consider all sources of carbohydrates (dextrose containing IV fluids, oral intake, medications).
- Carbohydrate: <150 g/day or < 2 mg/kg/minute.
- Protein: start at the goal of requirements up to 1.5 g/kg.
- Supplementation: daily multivitamin and 100 mg thiamine × 3 days.
- Obtain bloodwork: replace low electrolyte levels (prior to initiating feeding, 4-6 hours after initiating feeding, and daily for minimum 5 days).
Carson’s Plan for Starting Enteral Nutrition
Carson is at risk for refeeding syndrome: start conservatively and advance nutrition slowly.
- Liaise with team to replace low electrolytes: K+ (3.3), PO4 (0.7) – prior to initiation of enteral feeds and 6 hours after. Ensure electrolytes are ordered daily × 5 days and monitor for further replacements
- Liaise with team to order: multivitamin (daily) and 100 mg thiamine (for 3 days)
- Starting rate: Isosource 1.2 @ 25 mL/hr × 20 hrs (holding 2hrs pre & post Levothyroxine administration)
- Starting rate provides: 600 kcal (10 kcal/kg), 27 g protein/day (0.46 g/kg), 78 g CHO/day – these amounts align with guidelines for refeeding syndrome
- Progression: if tolerated × 24 hrs, increase 10 mL q 12 hrs to goal rate of 75 mL/hr × 20 hrs
Carson’s Protein Needs
In Carson’s case, the amount of protein he is receiving when initiating enteral feeds is low.
Based on the current plan, Carson will not meet his goal rate until ~day 3 of enteral feeding (this is if there are no complications/interruptions to progressing towards goal). It may be worthwhile to incorporate additional protein (Beneprotein®) until the goal rate is reached. Beneprotein is a protein module (1 = 25 kcal & 6 g protein).
- Starting protein intake: 27 g/day from Isosource 1.2 @ 25 mL/hr × 20 hrs/day.
- Estimated protein requirement: 1.2 g/kg = 71 g/day (aim for lower end of target range).
- Protein deficit: 71 g requirement − 27 g from feeds = 44 g to meet 1.2 g/kg.
- Calculation: 44 g ÷ 6 g per pkg = 7 pkgs required (use 6 pkgs for nurse ease). 6 pkgs provides 150 kcal and 36 g of protein.
- Starting rate: Carson will receive 750 kcal (13 kcal/kg/day) and 63 g protein (1.1 g/kg/day) from feeds and Beneprotein.
- Order: Mix 2 pkgs of Beneprotein with 100 mL of water and administer via G-tube . Plan to discontinue or decrease Beneprotein when enteral feeds are near or at goal.
Summary of Carson’s Nutrition Care Plan
Review the final summary for Carson’s nutrition care plan before commencing the simulation activity below.
| Area of Concern | Recommendations |
|---|---|
| Enteral nutrition via G-tube |
|
| Medications and infusions |
|
| Laboratory values |
|
| Supplements |
|
| Diet |
|
Simulation Activity: Carson
Blood Urea Nitrogen
In the context of enteral and parenteral nutrition, patency refers to the degree of openness of a feeding tube (i.e. an unblocked tube is patent).
Nurse Practitioner
package
Common medical abbreviation for Latin "ter in die" meaning "three times a day"

