Parenteral Nutrition
Plan
Page Contents
Team Rounds

Photo by Madailein Abbott is licensed under Public Domain.
Poppy’s PN Plan
When a dietitian is asked to assess a patient for PN, the first question should be “Is PN appropriate for this patient?” PN is an invasive, expensive and high-risk treatment compared to other methods of feeding.
In making your decision, consider the following about Poppy:
- She is not tolerating EN.
- She is critically ill (catabolic), with an acute kidney injury, and has lost a significant amount of weight preoperatively.
- Her history of severe PVD may contribute to a prolonged period of poor tolerance to enteral nutrition.
These factors coupled with inadequate nutrition support postoperatively may increase the chance of poor outcomes, morbidity and mortality.
Therefore, Poppy is appropriate for parenteral nutrition support.
Timing of PN Initiation
Initiation of parenteral nutrition may differ based on clinical indication and severity of malnutrition. It is common practice to initiate PN sooner for patients who are malnourished and are unable to meet their estimated nutrition requirements with oral intake or enteral nutrition. Other factors may also influence initiation of PN. However, general guidelines regarding initiation of PN are listed below.
- For well-nourished, stable patients: Initiate parenteral nutrition after 5 to 7 days if unable to receive > 50% of estimated requirements orally or enterally.
- Patients who are nutritionally-at-risk and unlikely to achieve adequate oral or enteral intake: Initiate parenteral nutrition within 3 to 5 days.
- In patients with baseline moderate or severe malnutrition and insufficient or unattainable oral or enteral intake: Initiate parenteral nutrition as soon as possible.
- For patients with severe metabolic instability: Delay initiation of parenteral nutrition until their condition has improved.
Reminder of PN Formulations
Macronutrients
The energy that is provided from macronutrients in PN is slightly different than the energy provided in other forms of nutrition (i.e. enteral formulas, food, beverages). Please note the differences below and ensure you use the correct values when determining your PN care plan.
Caloric contributions of macronutirients:
- Protein: 1 g amino acid = 4.0 kcal
- Carbohydrate: 1 g dextrose = 3.4 kcals
- Lipid: 1 g lipid = 10 kcals
Lipids
Depending on your hospital formulary, you may have access to various lipid emulsions. These emulsions vary in omega-3, 6 and 9 content. You should seek further readings regarding the use of various lipid emulsions and the associated advantages, disadvantages, and possible situations that they may be used in.
- Intralipid: made of safflower or soybean oil + glycerol emulsifier + phospholipid (egg) and available as 10%, 20% & 30%
- SMOFlipid: soybean oil, medium chain triglycerides (MCT), olive oil, and fish oil (6%/6%/5%/3% w/v)
- Omegavan: purely fish oils, DHA, EPA
- ClinOleic: olive oil
| Lipid Emulsions | Omega-3 | Omega-6 | Omega-9 | Saturated | MCT |
|---|---|---|---|---|---|
| Soybean oil emulsion | 5% | 60% | 20% | 15% | – |
| Olive-soybean oil mixture | 3% | 20% | 60% | 17% | – |
| Fish oil emulsion | 60% | 10% | 10% | 20% | – |
| SMOF emulsion | 10% | 20% | 30% | 10% | 30% |
Micronutrients
Vitamins, minerals, and trace elements should be included in parenteral nutrition solutions as depletion of a compromised patient’s micronutrient reserves could impair the patient’s ability to absorb and utilize nutrients.
Electrolytes are also added to PN solutions. Unlike vitamins, minerals and trace elements, electrolytes must be adjusted daily in a patient who is starting PN to account for losses, disease effects and organ function.
There are guidelines which govern how much calcium and phosphorus can be given to avoid precipitates. Acetate is added to buffer acid from amino acids as bicarbonate cannot be added. Large electrolyte deficiencies must be corrected by IV boluses (ordered by the MD/NP) prior to initiating PN or advancing solutions. Institutional formularies will determine which micronutrients are available and training should be provided to ensure safe delivery to patients.
Here is a sample electrolyte regimen for a stable patient receiving PN:
- Na: 80 – 120 mmol/day – with chloride, acetate
- K: 40 – 80 mmol/day – with chloride, phosphate or acetate
- Mg: 10 – 15 mmol/day – as sulfate salt
- PO4: 8 – 16 mmol/day – with Na or K
PN Procurement
PN is compounded in hospital pharmacy. Solutions may be individualized or standardized formulas, depending on the institution.
There are two types of PN procurement:
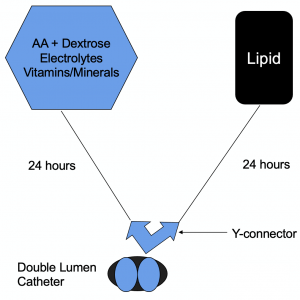
- “3-in-1” AA/dextrose/lipid/electrolytes in one bag
- “2-in-1” AA/dextrose/electrolytes + lipid in a separate bag.
Some hospitals have a pre-determined standardized formulary for ease of ordering and preparing PN. The pre-determined formulas are all named and vary in macronutrient volumes. Additives are individualized based on patients’ needs. The RD chooses the solution which closely matches the patient’s requirements. Here is an example of a standardized bag order form: Sample PN Formulary (PDF).
Some hospitals have individualized formulas which are prepared for a specific patient. If the hospital has a variety of solutions available, the RD can customize the PN formula to very closely match a patient’s estimated requirements. If there is a limited number of solutions, the PN formula may not be ideal to meet each estimated requirement.
It is possible that some hospitals may have both standardized and individualized formularies. If a standardized formula is not appropriate, the RD would calculate a custom solution.
PN Administration
When a patient is started on PN, it generally takes about 2 – 4 days to achieve goal volumes while monitoring metabolic tolerance. However, this may differ for specific patients:
- Patients who are very malnourished or show signs and symptoms of refeeding syndrome may take up to 7 days to safely receive goal volumes. Electrolytes, fluid and dextrose may need several steps of adjustment before a patient receives their goal nutrition provision.
- For patients who have diabetes or elevated blood glucose levels, it may take several days to adjust the patient’s insulin regime for acceptable glycemic control.
It is common for routine bloodwork to be drawn to monitor metabolic tolerance pre-PN and day 1, 2, 3 after starting PN. Typically after a patient has been stable on their goal volume of PN, bloodwork is drawn once or twice a week according to the institution’s protocol (unless the patient’s medical condition requires a different monitoring schedule).
When starting PN, it is usually given over 24 hours. Patients who require long-term PN have their delivery cycled to fewer hours to provide freedom from the IV pump/pole and improve quality of life (QOL). PN would be given over 20 hours a day, followed by 16 hours a day, followed by 12 hours a day.
Poppy’s Parenteral Regime: Formula Selection
Take note of Poppy’s estimated requirements:
- Weight: 63 kg
- Energy: 1575-1890 kcals/day
- Protein: 76-95 g/day
- Fluid: very conservative
The first step in determining Poppy’s parenteral plan is to select a solution. As mentioned, depending on your hospital, you will have access to different amino acid, dextrose and lipid solutions. In this case, we have access to a 5% amino acid solution, and varying dextrose solutions of 10%, 16.6%, and 25%. You can determine the energy content of each TPN solution by calculating the gram amount of amino acid and dextrose in 1L of solution. Depending on your patients needs, you can select a less or more concentrated solution.
Pause and consider which of the solutions you would choose, based on Poppy’s requirements:
- 5% amino acid (aa) + 10% dextrose (dex)
- 50 g aa × 4 kcal/g = 200 kcal
- 100 g dex × 3.4 kcal/g = 340 kcal
- 1 L TPN = 540 kcal
- 5% amino acid + 16.6% dextrose
- 50 g aa × 4 kcal/g = 200 kcal
- 166 g dex × 3.4 kcal/g = 564 kcal
- 1 L TPN = 764 kcal
- 5% amino acid + 25% dextrose
- 50 g aa × 4 kcal/g = 200 kcal
- 250 g dex × 3.4 kcal/g = 850 kcal
- 1 L TPN = 1050 kcal
When starting to work through your patient’s parenteral nutrition plan, it is common to start with calculating protein requirements. Clinicians use various methods to calculate a PN regime, however protein requirements are often a key factor and it is important to meet the patients needs. Therefore, it is suggested that you start by determining a solution that meets Poppy’s estimated protein requirements to avoid redoing your calculations multiple times.
Protein calculations
- 76 g needed ÷ 50 g (in 1 L) = need 1.52 bags = 1.52 L
- 1.52 L = 50 g aa × 1.52 = 76 g pro × 4 kcal/g = 304 kcal
If Poppy requires a minimum of 76 g of protein per day, this would require 1.52 L of TPN using a 5% amino acid solution. Protein will contribute 304 calories.
Carbohydrate calculations
- 100 g dex × 1.52 = 152 g CHO × 3.4 kcal/g = 517 kcal
- 166 g dex × 1.52 = 252 g CHO × 3.4 kcal/g = 859 kcal
- 250 g dex × 1.52 = 380 g CHO × 3.4 kcal/g = 1292 kcal
Based on Poppy’s needs, it is reasonable to choose the 16.6% dextrose solution.
This dextrose solution will contribute 859 calories in 1.52 L of the solution.
Lipid calculations
- Determine calories from lipid: 1700 kcal/day = 1700 − (304 from protein + 859 from CHO) = 537 kcal needed from 20% lipid
- Determine mL of lipid: 537 kcal/2 kcal/mL (20%) = 269 mL 20% lipid
- Determine grams of lipid: 537 kcal/10 kcal/g = 54 g lipid
In this case, we want to have a greater caloric contribution from lipid because Poppy’s fluid requirements are restricted. Including a higher amount of lipid results in a more fluid restricted solution as lipids are calorically dense.
Poppy will receive 537 calories from lipid to meet her needs of approximately 1700 calories a day from TPN.
Practice these calculations and review the answers.
Poppy’s Parenteral Regime: Summary of Formula Selection
Here is a summary of the formula based on 5% amino acid, 16.6% dextrose, 20% SMOFlipid and standard electrolytes.
The total amount of fluid is 1789 mL to meet Poppy’s energy needs of 1700 calories a day.
Keep in mind that you would have need to liaise with the physicians on your team to approve the fluid volume of your TPN order as they have requested that you minimize Poppy’s fluid intake.
5% amino acid / 16.6% dextrose + 20% SMOFlipid + standard electrolytes + MVI
- 1.52 L 5% amino acid / 16.6% dextrose
- 76 g pro / 304 kcal
- 252 g CHO / 859 kcal
- 269 mL 20% SMOFlipid
- 54 g fat / 537 kcal
Total: 1789 mL (1520 mL dextrose and AA + 269 mL lipid) / 1700 kcal
Macronutrient Tolerance and Distribution
| Macronutrient tolerance | Macronutrient distribution | |
|---|---|---|
| Dextrose | < 4-5 mg/kg/min | 45 – 65% |
| Lipid | ≤ 2.0-2.5 g/kg/day (<1.5 g/kg/day preferred) or < 30% of daily kcal | 10 – 35% |
| Protein | As per estimated requirements | 10 – 35% |
Poppy’s Parenteral Regime: Macronutrients
Poppy’s Estimated Requirements
- Weight: 63 kg
- Energy: 1575-1890 kcal/day
- Protein: 76-95 g/day
- Fluid: very conservative
- Protein as per estimated requirements: 76 g/63 kg = 1.2 g/kg
- Lipid ≤ 2.0-2.5 g/kg/day: 54 g fat/63 kg = 0.86 g/kg
- Dextrose ≤ 4-5 mg/kg/min:
- 252 g dextrose = 252000 mg
- 252000 mg/63 kg/1440 min = 2.8 mg/kg/min
For macronutrient tolerance, protein is 1.2 g/kg which is appropriate on initiation but may need to be adjusted depending on Poppy’s clinical status. Poppy would be receiving 0.86 g/kg of lipid, and 2.8 mg/kg/min of dextrose which is within the guidelines for macronutrient tolerance. In this case, the formula remains appropriate for Poppy.
Macronutrient distribution
- Protein = 304 kcal ÷ 1700 kcal × 100 = 18%
- Carbohydrate = 859 kcal ÷ 1700 kcal × 100 = 51%
- Fat = 537 kcal ÷ 1700 kcal × 100 = 32%
The macronutrient distribution of Poppy’s PN solution is 18% protein, 51% carbohydrate, and 32% fat — all are within the recommended ranges. The amount of protein Poppy will be receiving is on the lower end of the range and the amount of fat she will be receiving is on the higher end of the range. This is acceptable as a limited number of PN solutions are available on our formulary and we are working to meet Poppy’s estimated protein requirements and limit total fluid volume. As fat is calorically dense we elected to increase her proportion of fat intake to reduce fluid intake. As with any nutrition care plan , Poppy’s estimated nutrition requirements will be re-evaluated periodically based on her clinical status and her PN solution may change.
Rate of Administration
- 5% amino acid + 16.6% dextrose: 1.52 L = 1520 mL ÷ 24 hrs = 63 mL/hour
- 20% lipid: 269 mL ÷ 24 hours = 11 mL/hour
- TFI: 1520 + 269 mL = 1789 mL/day (28mL/kg)
The last step when planning a parenteral nutrition regime is to calculate the rate of administration. Poppy will receive her “2 in 1” solution of amino acids and dextrose (plus additives) at 63 mL/hour and lipids at 11 mL/hour. This results in 1789 mL/day of fluid, which is 28 mL/kg. The ICU intensivist has approved this fluid volume.
Initiating PN & Refeeding Syndrome
When your patient is at risk of refeeding syndrome, you should:
- Initiate feeding as soon as possible
- Determine caloric and protein requirements using current weight
- Start nutrition slowly via continuous infusion
- Energy: no more than 50% of energy requirements in the first 24 hours, maximum 15-20 kcal/kg (if at severe risk: ≤10 kcal/kg).
- Carbohydrate: <150 g/day or < 2 mg/kg/minute. Consider all sources of carbohydrates (dextrose containing IV fluids, oral intake, medications).
- Protein: start at the goal of requirements up to 1.5 g/kg.
- Supplementation: daily multivitamin and 100 mg thiamine × 3 days.
- Obtain bloodwork: replace low electrolyte levels (prior to initiating feeding, 4-6 hours after initiating feeding, and daily for minimum 5 days).
Poppy’s Parenteral Regime: Refeeding Syndrome
As per our assessment, Poppy is at low-moderate risk of refeeding syndrome.
Despite the refeeding risk, PN is initiated conservatively to assess metabolic tolerance. The conservative start typically meets the requirements for safely starting nutrition support when a patient is at risk of refeeding syndrome.
Request thiamine and multivitamin supplementation for patients who are at risk.
Summary of Nutrition Plan
Summary of Poppy’s Nutrition Care Plan
| Area of Concern | Recommendations |
|---|---|
| Parenteral Nutrition |
|
| Medications and Infusions |
|
| Laboratory Values |
|
| Supplements |
|
| Diet |
|
Simulation Activity: Poppy
PART 2: PLAN COMPLETE. Pause to reflect on the nutrition care plan we created for Poppy. When you’re ready, move on to Part 3: Implementation.

