Inpatient GI
Background
Page Contents
Conditions Covered in this Section
This “Background” section of the Inpatient GI module addresses three main conditions:
- Inflammatory Bowel Disease (IBD)
- Ostomies
- Pancreatitis
After reviewing background information, you will be led through the Nutrition Care Process along with a relevant case study to apply your knowledge. The case study will be a complex case focused on IBD and ostomies. A summary of evidence, education, and recommendations will be provided for all topics.
It may also be useful to review the first section of the Background for Outpatient GI, which provides a general overview of GI system components, digestion, and nutrient absorption.
Inflammatory Bowel Disease (IBD)
Symptoms may include severe diarrhea (with blood and mucus), abdominal pain, fatigue, malabsorption of nutrients, anemia, and weight loss. As a result, IBD disrupts the body’s ability to digest food, absorb nutrients and eliminate waste. It is estimated that up to 85% of hospitalized IBD patients have protein energy malnutrition, based on abnormal anthropometric and biochemical parameters.
Although specific causes of IBD are yet to be discovered, there are risk factors associated with IBD:
- Age: Most people who develop IBD are diagnosed before they’re 30 years old. Some people don’t develop the disease until their 50s or 60s.
- Ethnicity: Caucasian’s have the highest risk of the disease; but it can occur in any race.
- Family history: You’re at higher risk if you have a close relative, such as a parent, sibling or child with the disease.
- Cigarette smoking: Cigarette smoking is the most important controllable risk factor for developing Crohn’s disease. Although smoking may provide some protection against ulcerative colitis, the overall health benefits of not smoking make it important to try to quit.
- Non-Steroidal anti-inflammatory medications (NSAIDs): These include ibuprofen (Advil, Motrin), naproxen sodium (Aleve), diclofenac sodium (Voltaren) and others. These medications may increase the risk of developing IBD or worsen disease in people who have IBD.
- Where you live: If you live in an industrialized country, you’re more likely to develop IBD. Therefore, it may be that environmental factors, including a diet high in fat or refined foods, play a role. People living in northern climates also seem to be at greater risk.
Some of these are modifiable risk factors (such as cigarette smoking), while other factors are fixed (such as family history and ethnicity). It is important to note that diet and stress do not cause IBD, but still play a role in aggravating symptoms for those diagnosed.
Comparing Crohn’s Disease and Ulcerative Colitis
Crohn’s Disease is a chronic inflammatory disease that may involve any area throughout the entire digestive tract — anywhere from the mouth to the anus. However, it often affects the terminal ileum within the small intestine. Inflammation can extend through the entire thickness of the bowel wall, resulting in diarrhea, strictures, anal fissures, abscesses and fistulas.
Ulcerative Colitis is an inflammatory disease that begins at the anus and involves the inner mucosa of the colon. The inflammation does not result in fistulas, although extensive inflammation may require surgery to remove affected area. Ulcerative proctitis, a milder form of UC, occurs at a maximum of 20 cm proximal to the anus.
Complications in common
Ulcerative colitis and Crohn’s disease have some complications in common and others that are specific to each condition.
Complications found in both conditions may include:
- Colon cancer: having IBD increases your risk of colon cancer. General colon cancer screening guidelines for people without IBD call for a colonoscopy every 10 years beginning at age 50. For those with IBD, this test may need to be done sooner and more frequently.
- Skin, eye and joint inflammation: Certain disorders, including arthritis, skin lesions and eye
inflammation (uveitis), may occur during IBD flare-ups. - Medication side effects: Certain medications for IBD are associated with a small risk of developing certain cancers. Corticosteroids can be associated with a risk of osteoporosis, high blood pressure and other conditions.
- Primary sclerosing cholangitis: In this condition, inflammation causes scars within the bile ducts, eventually making them narrow and gradually causing liver damage.
- Blood clots: IBD increases the risk of blood clots in veins and arteries.
Complications of Crohn’s Disease
The complications specific to Crohn’s disease are related to the deeply-penetrating nature of the inflammation, as well as its ability to affect any spot along the digestive tract. The severity and recurrence of complications is variable.
- Bowel obstruction: Crohn’s disease affects the full thickness of the intestinal wall. Over time, parts of the bowel can thicken and narrow, which may block the flow of digestive contents. Patient’s may require surgery to remove the diseased portion of the bowel.
- Malnutrition: Diarrhea, abdominal pain and cramping may make it difficult to eat or for the intestine to absorb enough nutrients to keep the patient nourished. It’s also common to develop anemia due to low iron or vitamin B12 caused by the disease.
- Ulcers: Chronic inflammation can lead to open sores (ulcers) anywhere in the digestive tract, including the mouth and anus, and in the genital area (perineum).
- Fistulas: Sometimes ulcers can extend completely through the intestinal wall, creating a fistula — an abnormal connection between different body parts. Fistulas near or around the anal area (perianal) are the most common kind. In some cases, a fistula may become infected and form an abscess.
- Anal fissure: This is a small tear in the tissue that lines the anus or in the skin around the anus where infections can occur. It’s often associated with painful bowel movements and may lead to a perianal fistula.

Complications of Ulcerative Colitis
Ulcerative Colitis may appear to have fewer complications than Crohn’s, but it is important to remember that the inflammation may still require surgery, ultimately affecting nutrient absorption and increasing malnutrition risk. These complications can be life-threatening if not addressed.
- Toxic megacolon: Ulcerative colitis may cause the colon to rapidly widen and swell, a serious condition known as toxic megacolon.
- Severe dehydration: Excessive diarrhea can result in dehydration
Factors Altering Nutritional Status
There are many factors that can impact an individual’s nutrition status in IBD. They may increase someone’s risk of malnutrition, affect their ability to access or prepare food, and change their anthropometric data.
Review the following factors and identify which are more closely related to Crohn’s, Ulcerative Colitis, or both.
- Decreased nutrient intake
- Severe diarrhea
- Blood in stool
- Abdominal pain and cramping
- Fatigue
- Weight loss
- Nausea and vomiting
- Restrictive diets
- Side effects of medications (appetite suppression, taste alterations)
- Mouth sores
- Increased needs for healing (protein, vitamins and minerals)
- Malabsorption
- Surgical resections
Treatment Options
Treatment for IBD falls into two main categories: medications and surgery. Drugs are primarily used to manage symptoms of IBD and reduce inflammation, the most common of which are explored in the “Medications” section below. Crohn’s disease is more likely to require surgical treatment, with around 70% of individuals affected undergoing ileostomy or bowel resection. The complications of each GI surgery are listed in the “Surgery” section below.
Medications
The tables below provide an overview of medications used to reduce inflammation and manage symptoms of patients with IBD.
| Medications | General Explanation | Examples |
|---|---|---|
| Sulfasalazine and 5-Aminosalicylates (5-ASA) | These drugs limit the production of certain chemicals that trigger inflammation. This medicine is generally prescribed to help combat milder attacks of Crohn’s or UC. | Mesalamines, Sulfazine |
| Steroids | Steroids aim to reduce inflammation. These drugs are used by patients who have moderate to severe attacks. | Prednisone, Hydrocortisone |
| Immunomodulators | This type of medicine alters how the body mounts an inflammatory response. Immunomodulators do supress the ability to fight infections in general. These drugs are used by patients who have moderate to severe attacks. | Methotrexate |
| Biologics | These drugs target and block molecules involved in inflammation. These drugs are used to combat moderate to severe attacks. | Adalimumab (Humira)
Infliximab (Remicase, Inflectra) Vedolizumab (Entyvio) Ustekinumab (Sterlara) |
| Antibiotics | Antibiotics do not counteract inflammation directly but decrease infection that can cause severe inflammation. | Ciprofloxacin, Metronidazole |
| Medications | General Explanation | Examples |
|---|---|---|
| Antidiarrheals | Used to treat diarrhea and works by slowing down the movement of the gut. Relieves symptoms of increased frequency and urgency. | Loperamide, Diphenoxylate, Cholestyramine |
| Antispasmodics | Relieves, prevents or lowers the incidence of muscle spasms. | Hyoscyamine, Dicyclomine |
| Bulk formers | Soak up water in the stool, thereby firming it up as well as reducing frequency. | Fybogel, Normacol |
| Bile salt binders | Prevent irritation of the gut by capturing bile salts. | Cholestyramine, Colestipol |
| Stool softeners | For softening feces to ease bowel movements. | Docusate |
| Analgesics | For pain reduction | Acetaminophen, Morphine, Hydrocodone, Oxycodone |
| Non-steroidal anti-inflammatory drugs (NSAIDs) | For pain control in joints (Note: some people find these drugs aggravate their abdominal pain and diarrhea). | Aspirin, Ibuprofen, Naproxen |
| Acid reducing drugs | For “heartburn” | Cimetidine, Famotidine, Nizatidine |
Surgery
Approximately 70% of people with Crohn’s and 40% of those with Ulcerative Colitis will require surgery at some point in their lives. Surgery should not be regarded as a last resort, it is simply another treatment option. The most common types of surgeries for people with IBS are ileostomies or primary resection.

The table below summarizes nutrition complications after GI surgery, depending on the type of resection.
| Type of Resection | ↑TG | ↑BG | Fluid/ electrolyte balance | GI Function | Malabsorption | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Gastroparesis | Anastomotic Leak | Chyle Leak | Dumping Syndrome | Fat | Vitamin | Mineral | ||||
| Esophagastric | X | X | X | X | ||||||
| Gastric | X | X | X | X | B12, D | Fe, Ca | ||||
| Pancreas | X | X | X | X | X | X | X | A, D, E, K, B12 | Fe, Ca, Zn | |
| Hepatocellular | X | X | X | X | A, D, E, K, B12, Folic acid | Mg, Zn | ||||
| Gall Bladder | X | X | X | X | X | A, D, E, K, B12 | Fe, Ca, Zn | |||
| Bile Duct | X | X | X | X | A, D, E, K, B12 | Fe, Ca, Zn | ||||
| Small Bowel | X | X | X | X | X | A, D, E, K, B12 | Fe, Ca, Zn | |||
| Colon or Rectum | X | X | B12 | Na, K, Mg, Ca | ||||||
Ostomies
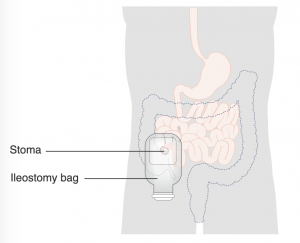
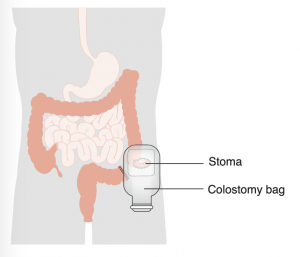
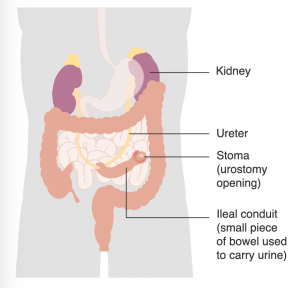
An ostomy is a change in the way urine or stool exits the body as a result of a surgical procedure. Bodily waste is rerouted from its usual path because of malfunctioning parts of the urinary or digestive system. An ostomy can be temporary or permanent.
A stoma is the opening created by the ostomy surgery. It is located on the abdomen and is dark pink in color. For most ostomies, a pouch is worn over the stoma to collect stool or urine. For some people it is possible to have a continent diversion, an alternative to a conventional ostomy that eliminates the necessity for a pouch.
The three most common forms of ostomies are ileostomies, colostomies, and urosomies.
Ileostomy: A surgically created opening from the ileum, the lowest part of the small intestine. The intestine is brought through the abdominal wall to form a stoma. Ileostomies may be temporary or permanent, and may involve removal of all or part of the colon.
Colostomy: The surgically created opening of the colon (large intestine) which results in a stoma. A colostomy is created when a portion of the colon or the rectum is removed, and the remaining colon is brought to the abdominal wall. It may further be defined by the portion of the colon involved and/or its permanence.
Urostomy: This is a general term for a surgical procedure which diverts urine away from a diseased or defective bladder. The ileal or cecal conduit procedures are the most common urostomies. Either a section at the end of the small bowel (ileum) or at the beginning of the large intestine (cecum) is surgically removed and relocated as a passageway for urine to pass from the kidneys to the outside of the body through a stoma.
Pancreatitis
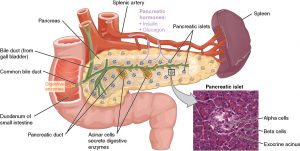
The pancreas is an important gland in the digestive system, located behind the stomach in the upper abdomen.
There are two main functions of the pancreas:
- Exocrine, which makes digestive enzymes
- Enzymes such as amylase, lipase and gastric juices help to digest food
- The pancreas releases enzymes into progressively larger ducts towards the main pancreatic duct
- The enzymes then drain into the duodenum
- Endocrine, which makes hormones
- The Islets of Langerhans make insulin and glucagon
- These hormones are released into the blood stream to control blood sugar (glucose) levels
Pancreatitis is inflammation in the pancreas. Pancreatitis occurs when digestive enzymes become activated while still in the pancreas, irritating the cells of your pancreas and causing inflammation. With repeated bouts of acute pancreatitis, damage to the pancreas can occur and lead to chronic pancreatitis. Mild cases of pancreatitis may go away without treatment, but severe cases can cause life-threatening complications. Risk factors include excessive alcohol consumption, cigarette smoking, obesity and family history.
Pancreatitis can occur as acute pancreatitis, meaning it appears suddenly and lasts for days; or as chronic pancreatitis, which occurs over many years.
Acute Pancreatitis
Signs and symptoms of acute pancreatitis include upper abdominal pain, fever, rapid pulse, nausea, and vomiting.
Many causes of acute pancreatitis exist, with biliary stones and alcohol overuse causing around 70-80% of cases. Obstructive causes like gallstones and tumours may also occur. Gallstones can get stuck in the common bile duct and press on the pancreatic duct, which blocks normal flow and leads to pancreatic injury. Other causes can include: toxins such as scorpion bites, certain drugs (ex. azathioprine), trauma from surgical procedures or blunt trauma, and infections (viruses, bacteria, parasites). Metabolic causes for acute pancreatitis include hypertriglyceridemia and hypercalcemia.
- Mild acute pancreatitis: No organ failure, local or systemic complications
- Moderately severe acute pancreatitis: Transient organ failure > 48 hours, local complications
- Severe acute pancreatitis: Persistent organ failure > 48 hours, local complications
- Necrotizing acute pancreatitis: Inflammation associated with necrosis (death) of the pancreas or surrounding tissues (increased risk of death by 36-50%)
Initial treatment in the hospital for acute pancreatitis involves various management strategies.
Fasting is indicated to allow the pancreas to recover. Once the inflammation in the pancreas is controlled, the patient will typically be switched to clear fluids and eating bland foods. With time, they can go back to a normal diet.
As pancreatitis can cause severe pain, pain medications are often used. The health care team will give the patient medications to help control the pain. Dehydration is also likely. For this reason, individuals typically receive extra fluids through intravenous route (IV).
Treatment of the underlying cause will range based on the patient’s circumstances and needs. This could include surgery, medications, or education (dietary, alcohol dependence, etc).
Chronic Pancreatitis
Nutrient malabsorption is one of the most common complications, related to pancreatic digestive enzymes. Specifically, vitamin B12 deficiency and fat-soluble vitamin deficiency can occur. The development of diabetes is also common, as pancreatitis damages the cells that produce insulin and glucagon. About 45% of people with chronic pancreatitis will develop diabetes.
Pseudocysts are another complication of chronic pancreatitis. These “cysts” are a collection of pancreatic fluid caused by direct leakage from the inflamed gland or the pancreatic duct. About 50% of pseudocysts resolve on their own. Treatment may be necessary when they become symptomatic, infected, or are increasing in size.
Treatments of chronic pancreatitis may have similarities to that of acute pancreatitis, such as with pain medications, and dietary education. Unique treatment approaches are also used, such as enzymes to improve digestion. Pancreatic enzyme supplements help the body break down and absorb the nutrients in food, and are taken with each meal. If the patient has autoimmune pancreatitis, steroids may be used. Surgery is not necessary for most people, but remains an option.

