Outpatient GI
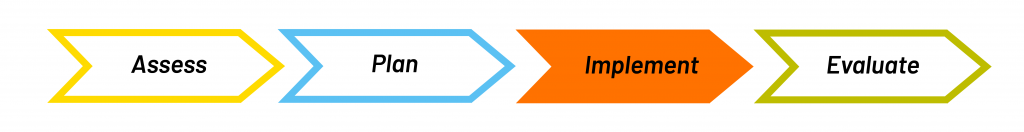
Implement
Page Contents
Interdisciplinary Team
When implementing your nutrition care plan, you may have to liaise with other members of the care team. You’ll want to discuss the clients treatment plans, if you have a suggestion or document a new findings after your appointment with the client. You may consider asking the client if they would want to see a particular professional (such as a social worker), if you feel it may benefit their care or a concern that is outside of your scope of practice. Review the different professions listed below.
- Physician or Nurse Practitioner: Assess patient needs, order and interpret lab work, diagnose, and prescribe treatment plans.
- Pharmacist: Advise on safe and effective medication to use for specific conditions and respond to patients symptoms by managing medications and their interactions.
- Social Worker: Provide counselling and identify sources of emotional support for patients and their families to cope with diagnoses or life stressors.
- Psychiatrist: Provide counselling to assess both mental and physical aspects of psychological problems. Specializes in the diagnosis, prevention, and treatment of mental disorders.
- Gastroenterologist: Provide specific treatment and diagnosis of GI problems and diseases. First they will assess and consult regarding the client. Often involved when exploring concerning symptoms or administrating testing. They may provide a diagnosis or opinion immediately, or order testing and bloodwork to determine a diagnosis.
Liaising with Christian’s Team
Regarding supplements
Christian is concerned about his iron and B12 values and is experiencing symptoms affecting his quality of life (i.e. headaches, fatigue, lightheadedness). He is interested in starting to incorporate a supplement, in hopes that it will contribute to a relief of his symptoms. He is open to exploring ways to improve this with diet in future appointments (e.g. exploring iron-rich foods), but for now he is most interested in supplements.
To address Christian’s concerns, you:
- Suggest the addition of an iron and vitamin B12 supplement
- Provide him with information on the potential GI side effects of iron (e.g. nausea, flatulence, abdominal pain, constipation, diarrhea, and black stools)
- Suggest updated lab work for Christian after 3-4 months (typical timeline) to reassess related lab values and the effectiveness of the supplement (i.e. is Christian lacking the appropriate amount of iron or is there a possible absorption issue?)
In this case, you do not need to directly liaise with the team on initiation of these supplements, but you would note the addition of them to the clients care plan. If not already initiated, you may request that his physician provides a laboratory requisition (during the established timeframe) so that you can properly evaluate the use of the supplements on your clients values.
Education
When implementing your plan with your client you may need to provide some education to them. When educating clients, try to:
- Individualize the education as much as possible: Discuss high-risk topic first since they are the priority, connect the client’s goals to your plan, and focus on what they want to learn.
- Find out if patient has had previous education: Ask the client if any one else has talked to them, and adjust your education accordingly.
- Focus on a few key messages: If the client is newly diagnosed or doesn’t know much about the management of GERD or IBS, try not to overwhelm them with too much information during your first couple of interactions. Instead give them a few small goals or suggestions to start.
Think of some key messages you might want to speak to Christian about when providing education.
Christian’s Education
Review the education statements below. These are examples of what you may speak with Christian about in regards to his nutrition care plan. However, you may have brainstormed additional statements outside of these.
| Area of Concern | Key Messages for Education |
|---|---|
| Medication and supplements |
|
| GERD & IBS Management |
|
| Dietary choices |
|
| Lifestyle habits |
|
Supporting Change
Prochaska and DiClemente’s transtheoretical model (also known as “stages of change”) can be a useful tool in assessing your client’s willingness to change. These “stages” can be used during charting and PES statements. The five stages are listed below with corresponding statements:
- Precontemplation: “I am not ready for change.”
- Contemplation: “I am intending to make changes in the next 6 months.”
- Preparation: “I am intending to make changes in the next month.”
- Action: “I have made changes in the last month and continue to make changes.”
- Maintenance: “I am managing my condition with my previous changes for more than 6 months.”
Ongoing management of a chronic disease can lead to burnout, and making dietary changes may be difficult for some clients. To help support them in making these changes, you may want to try:
- Motivational interviewing: collect their story, listen reflectively, collaborate rather than convince
- setting: help to identify barriers to change as part of creating a nutrition care plan with the client
- Referral to social worker: consider referring them to a social worker if they need someone to talk to about coping with the burden of managing a chronic disease
Christian’s SMART Goals
Here are some SMART goals Christian could work on based on his diet history and our nutrition care plan. When making SMART goals, you can discuss potential barriers and strategies to overcome those barriers. It is important to make Christian feel motivated and confident that he can achieve these goals, but if he does not, that is something you can work on with him.
- I will go to bed at 11:00pm instead of 12:00am every night starting next Sunday.
- I will limit myself to one cup of coffee per day starting next Sunday.
- I will have one glass of red wine every other night instead of daily starting next Sunday.
- I will remove tomatoes, onions, garlic, cabbage, and spices from my diet for the next two weeks starting next Sunday.
- I will eat my lunch spread out over 30 minutes instead of 15 minutes starting next Sunday.
- I will keep a food journal documenting what I eat, drink, my environment, my symptoms and my bowel movements for two weeks starting next Sunday.
Goals that are Specific, Measurable, Achievable, Relevant, and Time-bound.

