Hypertension and Dyslipidemia
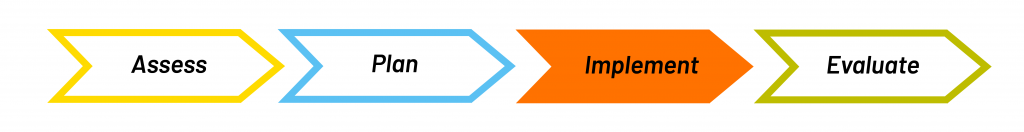
Implement
Page Contents
Supporting Change
Ongoing management of a chronic disease can lead to burnout, and making dietary changes may be difficult for some patients. To help support them in making these changes, you may want to try:
- Motivational interviewing: collect their story, listen reflectively, collaborate rather than convince.
- setting: help to identify barriers to change as part of creating a nutrition care plan with the client.
- Referral to social worker: consider referring them to a social worker if they need someone to talk to about coping with the burden of managing a chronic disease.
David’s SMART Goals
As outlined in the Part 2, there are a number of things David can work on as part of his nutrition care plan. Out of those recommendations you work together with him to decide on what to focus on and create these 5 SMART goals to achieve outcomes of reduced cholesterol and BP. As a part of making the goals SMART, you can discuss with him when he plans on making these changes by and come up with ways to support him if or when he encounters barriers.
Use the DASH Diet Recommendations to:
- Increase vegetable consumption by adding ½ cup extra vegetables to his soup 1 time per week starting next Monday.
- Reduce sodium by using the Nutrition Facts table to look for low sodium options when buying foods like canned soup when going grocery shopping this Thursday.
- Replace saturated fat intake with unsaturated fats by having lean meats, like chicken, or fish 2 times per week instead of beef and bacon starting tomorrow.
- Increase fibre by choosing whole grain bread instead of white bread and taking Metamucil once per day with lunch starting this Friday.
- Reduce alcohol consumption to 1 beer per day starting tomorrow.
Interdisciplinary Team
When implementing your nutrition care plan, you may have to liaise with other members of the care team. Ongoing management of a chronic disease can lead to burnout, and clients may need someone to talk to, like a social worker, about coping with this extra burden. Injury may be a barrier to initiating physical activity safely and comfortably, so they may benefit from talking to a physiotherapist or kinesiologist. You’ll want to discuss if you think a client might benefit from increasing or changing medications, and share successful outcomes. This may include liaising with the physician or nurse practitioner, or cardiologist or specialist. Read about the following roles in more detail if you are not familiar with them.
- Physician or Nurse Practitioner: Assess patient needs, order and interpret lab work, diagnose conditions, and prescribe treatment plans.
- Social Worker: Provide counselling and identify sources of emotional support for patients and their families to cope with CVD.
- Physiotherapist or Kinesiologist: Provide manual therapy and education related to movement and exercise to help people engage in physical activity.
- Cardiologist or Vascular Specialists: Specializes in diagnosing and treating diseases of the cardiovascular system. May carry out tests or perform procedures depending on CVD diagnoses.
Liaising With David’s Team
- In this case you have liaised with David’s physician regarding your suspicion that the new blood pressure medication may be contributing to constipation. You suggest adding in Metamucil as it may assist with relieving constipation and reducing cholesterol levels. The physician agrees with you.
- You also liaise with the physician regarding David’s lower back injury and suggest involvement of a physiotherapist, if and when David decides to start being physically active.
Education
When implementing your plan with your client you may need to provide some education to them about hypertension, dyslipidemia and nutrition. Like David, many clients may have no prior nutrition education. It is important to start with basic nutrition teaching, despite the need for specific disease-related teaching.
Here are some suggestions for starting a nutrition education plan with a client that has no prior nutrition education:
- Ask your client what they know: Never make an assumption that your client has an understanding of basic nutrition information (example, the three types of macronutrients).
- Start with the basics: Even if the client is seeing you for specific disease-related information (i.e. hypertension), it is important to make sure they have a basic understanding.
- Use visuals and plain language to help convey your messages (e.g. props, resources, handouts). Try to offer resources in the client’s first language if you are able.
-
Be transparent about time restrictions and explain your plans for future sessions. You do not have to educate on everything in one counselling session. You can even make a plan with your client breaking down the topics you will cover at each session based on their goals.
-
Involve the client in the process as much as you can. This is a recommendation for the success of all clients; but for an individual who is making nutrition changes for the first time, it is important for motivation, confidence and enjoyment in the process.
-
Consider all clients are different. Some prefer education and understanding, while others want to be told what to do and are not interested in the detailed education. Ask them what they hope to get out of the counselling session so that you can provide them that.
Using Plain Language with David
An example of a message that you could discuss with David using plain language and visuals is how atherosclerosis occurs in the body, describing how blood flows through your arteries like water through a hose and can become clogged with plaque, making the artery walls thick and hard. Just like if you put your thumb over the end of a hose, the flow is restricted and pressure builds up.

- Blood flows through your arteries like water through a hose, delivering oxygen and nutrients to your body.
- Atherosclerosis occurs when your arteries become clogged with fatty deposits or plaque.
- Plaque is a sticky mixture of fatty streaks that build up, making the walls of the arteries thick and hard.
- Over time, the artery narrows or gets blocked, and this stops blood from flowing through the artery.
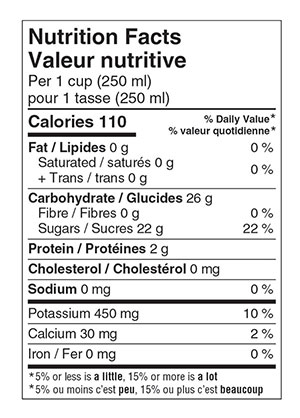
Education on Label Reading
Another important point to educate David on is label reading, including how to use the nutrition facts table and understand claims when grocery shopping for low sodium options.
Practice identifying the following details on the “Nutrition Facts” label pictured below:
- Serving Sizes: compare the serving size on the package to the amount that you eat.
- % Daily Value: shows you if a food has a little or a lot of a nutrient. For sodium, choose foods with a lower % DV: 5% or less is considered low in sodium, 15% or more is high.
- Claims about sodium: Beware! Sodium-reduced does not necessarily mean low sodium. Low in sodium means less than 140 mg sodium per serving. Salt-free means less than 5 mg sodium per serving.
David’s Education – Key Messages
Overall, to keep it simple focus on a these 5 key messages, asking questions throughout. It is also important to consider that David told you his wife does the cooking and grocery shopping. It may be worthwhile to suggest to David that he is welcome to bring his wife to future appointments so that she can receive the education too and learn about making healthy choices.
- Controlling your blood pressure, cholesterol, and triglycerides is important for reducing your risk for the development of other cardiovascular diseases.
- You can use the DASH Diet guidelines or CFG Healthy Plate to balance your meals and increase intake of vegetables.
- You and your wife can use food labels and the Nutrition Facts table to determine the amount of sodium in your food choices when grocery shopping.
- You can include unsaturated fats (fatty fish and nuts) more often than saturated fats (red meat and butter) to help control your dyslipidemia.
- You can take Metamucil and include more foods with whole grains by switching to whole grain bread from white bread.
Goals that are Specific, Measurable, Achievable, Relevant, and Time-bound.

