Parenteral Nutrition
Background
Page Contents
Nutrition Support Routes
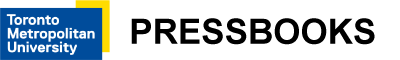
Nutrition support is the provision of enteral (EN) or parenteral nutrition (PN) to treat or prevent malnutrition. Nutrition support may be used to supplement oral intake. If the individual cannot eat, it can provide all of that individual’s nutritional requirements.
A basic flow diagram for assessment of nutrition support is presented below. This flow diagram can be impacted by a variety of variables but is a good representation of how to assess for enteral or parenteral nutrition. In consideration of more complex patients, you should use this diagram as a starting point for an assessment, not a comprehensive tool for decision making.
Parenteral Nutrition
Parenteral Nutrition (PN) refers to the infusion of an intravenous nutrition formula into the bloodstream as “parenteral” means “outside” or “alongside” the GI tract. Total Parenteral Nutrition (TPN) means that the infusion is an individual’s sole source of nutrition, meeting 100% of their estimated nutrition requirements.
Parenteral nutrition should be considered only when it is not possible to meet an individual’s nutritional requirements by the enteral or oral route. In such cases it may be necessary to bypass the gut and deliver nutrients directly into the bloodstream.
Sometimes parenteral nutrition may also be needed to supplement inadequate oral or enteral intake. This may occur where there is malabsorption (such as in short bowel syndrome or high output fistulas), or poor gut function (such as in intractable vomiting).
Benefits of PN include:
- Include provision of macronutrients, micronutrients and electrolytes
- Maintain weight and lean body mass
- Normalize electrolytes
- Reduce morbidity and mortality
- Improve clinical outcomes and quality of life
Risks of PN include:
- Infection,
- Altered liver function, hepatic steatosis, subsequent liver failure
- Line complications (pneumothorax, air embolus, subclavian artery injury, thrombophlebitis)
- Metabolic complications (hyperglycemia, hypertriglyceridemia, vitamin/mineral imbalances, electrolyte imbalances)
PN differs from EN in the following ways:
- Nutrients are provided via vein, bypassing the liver and gut
- There is a greater risk of complications (contamination, more invasive)
- Tolerance is greater
- There is less choice for formula (unless you have access to a compounder)
- Is it more expensive
- It requires continuous administration
- There is a need for daily revision
- There are more psychological effects
Nutritional Planning for PN
Making Decisions
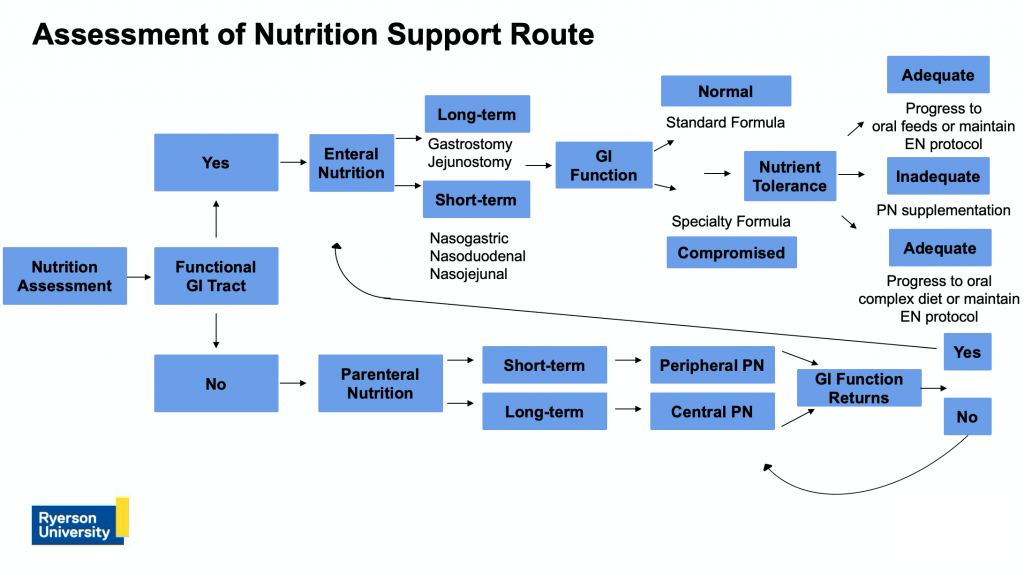
A basic flow diagram for parenteral nutrition planning is presented below. It can be used as a general assessment regarding considerations; however it can be affected by a variety of factors. This is where clinical judgment and expertise is required. Parenteral nutrition is often discussed in detail with the interdisciplinary team.
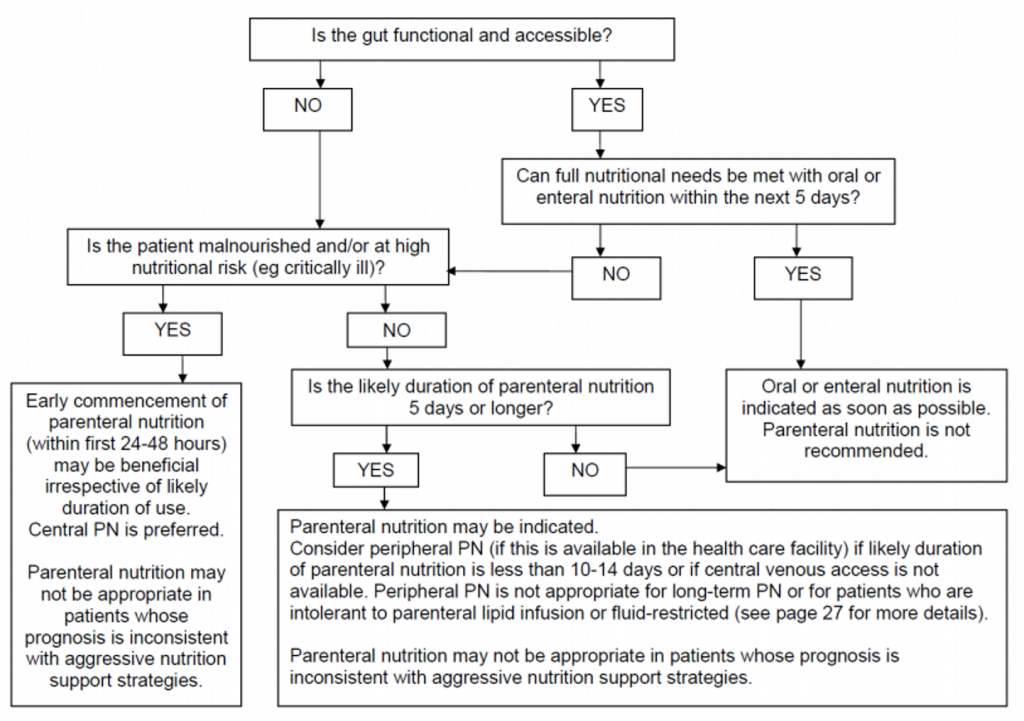
Figure. 2.3 Flowsheet for Nutrition Support Planning, From: Dietitians Association of Australia (2018), Parenteral nutrition manual for adults in health care facilities, Nutrition Support Interest Group, Retrieved Feb 25, 2022: https://dietitiansaustralia.org.au/wp-content/uploads/2018/06/Parenteral-nutrition-manual-june-2018-website.pdf This figure is being used under fair dealing for the purpose of education.
Assessing the Patient
When creating a parenteral nutrition plan, it is important to follow the general steps listed below.
- Determine requirements: energy, protein, and fluid.
- Check for risk of refeeding syndrome
- Determine route of PN: peripheral vs. central.
- Determine appropriate PN formula (amino acid/dextrose) to meet protein requirements: Calculate goal volume and rate. Dextrose (1 g = 3.4 kcal), Protein (1 g = 4.0 kcal).
- Provide remaining energy from lipid: Calculate goal volume and rate (1 g = 10.0 kcal for 20% lipid emulsions).
- Check macronutrient tolerance: dextrose (< 4-5 mg/kg/min), lipid (< 1 g/kg/day or < 30% of daily kcals), and protein (as per estimated requirements).
- Determine electrolyte requirements: determined based on labs/ requirements.
- Consider other additions:
- Trace elements: Site specific
- Multivitamin: Site specific
- Vitamin K: 2-4 mg per week if PN > 1 week
- Iron: Not routinely added, not recommended during acute illness or sepsis, may be needed for long-term/home PN patients
- Pantoprazole: Dose as per MD/Pharmacist (RPh), reduces acid secretion
- Zinc: Daily requirement of 2.5-5.0 mg/day, additional supplementation may be required with high volume stool, ostomy output, or to support wound healing
- Additional additives: Discuss with MD/RPh
Note that electrolyte requirements and other additives are very site specific. They also vary tremendously based on if the patient is critically ill, acutely ill or medically stable and if PN is expected to be short or long term. You should seek further readings or training regarding this.
Indications & Contraindications
Here is an overview of common indications for parenteral nutrition:
- Non-functioning GI tract or conditions precluding the use of the GI tract
- Pre-operative support of patients with moderate to severe malnutrition
- Severe acute exacerbations of Crohn’s disease or ulcerative colitis
- High output or proximal GI fistula
- Short bowel syndrome (< 100 cm)
- Severe acute necrotizing pancreatitis
- Complete bowel obstruction
- Prolonged paralytic ileus
- Mesenteric ischemia
- Anticipated requirement for > 7 days
In some cases, at the discretion of the medical team, a patient may receive PN for a reason not listed here. Review the list and look up any of the conditions that you are not familiar with.
Here is a list of the most common contraindications for patients who are being assessed to receive parenteral nutrition:
- Functioning GI tract
- Well-nourished and inadequate EN/oral diet for < 5-7 days
- Unstable hemodynamics
- Aggressive intervention not warranted/desired
Depending on your patient, the initiation of PN may be delayed if one of the above conditions is met. If the patient’s clinical course changes they may be appropriate to receive PN later in their admission. For example, an ICU patient becomes hemodynamically stable on day 3 and is appropriate to start PN.
Routes of Administration
Parenteral nutrition can be administered via peripheral or central line.
Peripheral PN
The access point for peripheral PN is via peripheral veins in the extremities (hands or feet).
Peripheral PN is used less commonly, as most hospitals prefer central access or patients do not meet the criteria to start PN. It is a short term solution with patients receiving peripheral PN for 10-14 days maximum with line changes q72hrs for line patency.
Peripheral PN is most useful:
- As supplemental PN
- As bridge therapy during transition periods (suboptimal oral intake/EN)
- In clinical circumstances where central IV access is not warranted
- While waiting for central IV access to be gained
The safe upper limit for osmolality is <900 mOsm/L. Higher volumes are needed to keep osmolality low and meet nutrition requirements.
There is an increased risk of phlebitis with peripheral PN and patients must have normal renal and cardiac function as well as normal lipid metabolism.
Central PN
The access point for central PN is via large vein (i.e. subclavian or vena cava).
Unlike peripheral PN, central PN can be used for any length of time and solutions can be higher osmolality (>1800 mOsm/L) due to high rate of blood flow, which dilutes the hypertonic solution.
Central PN can provide provision of full nutrient requirements, partial/ supplemental nutrient requirements and fluid restricted solutions.
PN can be administered to patients with poor renal and/or cardiac function or altered lipid metabolism via a central line.
Access Sites

Source: General Ludd, CC BY-SA 3.0 , via Wikimedia Commons
Parenteral nutrition is given into an intravenous access device, a fine silicon or polyurethane tube that is inserted into a vein.
Some intravenous lines contain multiple lumens — tiny separate tubes within the line — enabling several different solutions (including incompatible solutions) to be delivered at the same time.
Parenteral nutrition must be given into a lumen that is dedicated for that purpose. This means the lumen should not be used to give medications or anything other than nutrition. With a 2 in 1 solution, the amino acid/dextrose solution may need to be “Y connected” with the lipids to be infused into one lumen.
In the photo to the right, a two-lumen catheter is inserted on the patient’s left side. Scars at the base of the neck indicate the insertion point into the left jugular vein. The line runs under the skin over the collarbone to a point about seven centimeters below, where it emerges from the chest and splits into the two lumens. Each lumen has a clamp for closing off the line and each terminates with a threaded end for drawing blood for analysis, and attaching lines to infusion pumps, and apheresis and dialysis machines.
Peripheral Venous Access
Peripheral lines can be helpful in starting a patient on PN while they are waiting for central access. Peripheral lines are those that have their delivery tip outside the vena cava; the tip may lie in the subclavian or axillary veins in the upper arm or be a standard peripheral cannula in the basilic or cephalic veins of the lower arm. Solutions that can be used peripherally must be limited to < 900 mOsm/kg to minimize blood vessel damage. This means that peripheral parenteral nutrition solutions are usually a larger volume, more dilute solution, with a higher proportion of fat.
Peripheral parenteral nutrition is usually not recommended for patients who:
- are fluid-restricted
- have high protein requirements
- are intolerant to IV lipid infusion
- have high serum triglyceride levels
Advantages and disadvantages of peripheral lines
Adapted from Dietitians Association of Australia: Parenteral Nutrition Manual for Adults in Health Care Facilities (PDF).Type of Line Advantages Disadvantages Peripheral line - Quick and easy to insert
- Inexpensive
- Very low infection risk
- Usually requires rotation every 3 days due to vein inflammation
- Peripheral delivery limits the solution that can be used

Source: Blausen Medical Communications, Inc., CC BY-SA 4.0, via Wikimedia Commons (cropped from original)
Central Venous Access
All central venous access devices, by definition, have their delivery tip in the vena cava or right atrium. Different lines/devices will be inserted into different sites on the body, they vary in how long they can be used for, and how complicated the insertion/ removal methods are.
It is important to understand where these lines are inserted, the advantages and disadvantages to each, and to be able to identify what type of line it is when looking at a patient. A comparison and visual representation of common central venous access devices are depicted below.
| Type of Line | Advantages | Disadvantages |
|---|---|---|
| Peripherally-inserted central venous catheter (PICC) |
|
|
| Polyurethane short-term central line |
|
|
| Portacath |
|
|
Source: Blausen Medical Communications, Inc., CC BY 3.0, via Wikimedia Commons
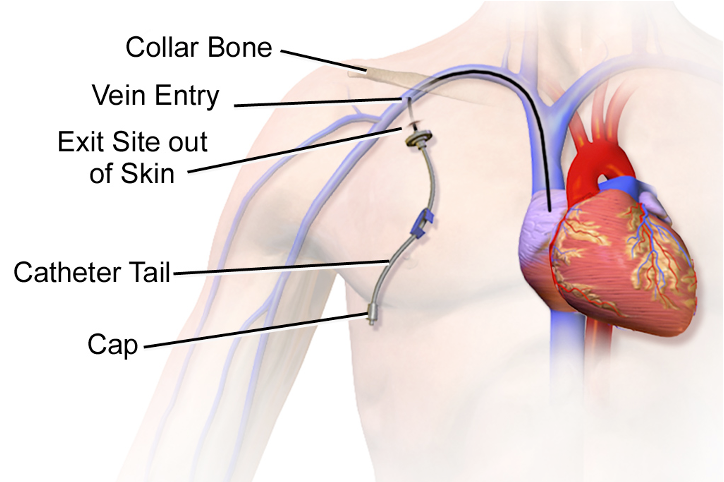
Source: Blausen Medical Communications, Inc., CC BY 3.0, via Wikimedia Commons (cropped from original)
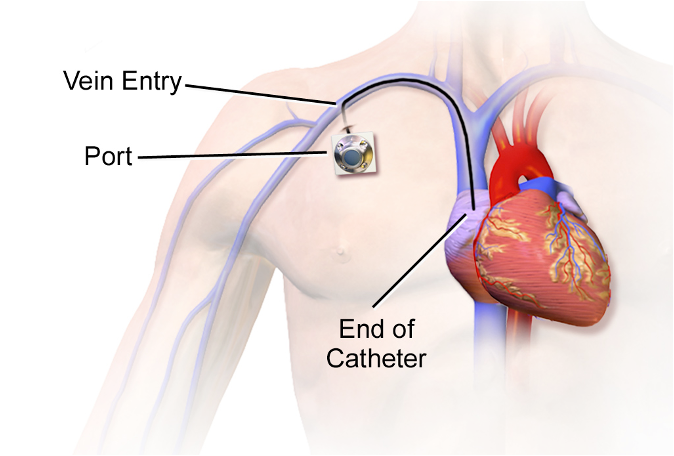
Source: Blausen Medical Communications, Inc., CC BY-SA 4.0, via Wikimedia Commons (cropped from original)
Macronutrients
The table below provides an overview of the macronutrients used in parenteral nutrition, along with a few key considerations for the use of each.
| Macronutrient | Explanation |
|---|---|
| Protein |
|
| Carbohydrate |
|
| Fat |
|
Micronutrients
Vitamins, minerals, and trace elements should be included in parenteral nutrition solutions as depletion of a compromised patient’s micronutrient reserves could impair the patient’s ability to absorb and utilize nutrients.
Patients who are starting on PN may require different micronutrient additions compared to patients who have been receiving long-term PN. Patients on long-term parenteral nutrition (longer than three to six months) need periodic monitoring of their micronutrient status as body stores may become depleted, even with supplementation, due to ongoing increased demands.
Depending on your hospital, you may be entirely responsible for determining micronutrients. In others, you may have a PN team where other team members (i.e. RPh/ MD) determine additives.
| Micronutrient | Examples |
|---|---|
| Water-soluble vitamins | Thiamine, Riboflavin, Niacin, Pantothenic acid, Vitamin B12, Folic acid, Vitamin C, and Biotin |
| Lipid-soluble vitamins | Vitamin A, Vitamin D, Vitamin E, and Vitamin K |
| Trace elements | Chromium, Copper, Iodide, Iron, Manganese, Selenium, Zinc, Fluoride |
Electrolytes
Electrolytes must be adjusted daily in a patient who is starting PN to account for losses, disease effects and organ function.
Large deficiencies must be corrected by IV boluses (ordered by the MD/NP) prior to initiating PN or advancing solutions.
Patients may continue to have fluctuating electrolyte levels throughout their admission as their clinical status changes, and may require IV electrolyte replacements even when stable on their goal solution of PN.
Stable patients or individuals who receive long-term PN will have different monitoring protocols/ requirements than those who are starting PN or acutely/critically ill.
Requirements for electrolytes may also be increased if the patient has increased losses, intracellular shifts or increased demand.
| Electrolyte | Daily requirements | Factors that increase needs |
|---|---|---|
| Sodium | 1 – 2 mmol/kg | Diarrhea, vomiting, GI losses |
| Potassium | 1 – 2 mmol/kg | Diarrhea, vomiting, medications, refeeding syndrome, GI losses |
| Calcium | 5 – 7.5 mmol/day | High protein intake |
| Magnesium | 4 – 10 mmol/day | Medications, refeeding syndrome, GI losses |
| Phosphorous | 20 – 40 mmol/day | High dextrose loads, refeeding syndrome |
Considerations in Choosing a PN Formulation
Here is a brief overview of additional considerations to take into account when choosing a parenteral nutrition formula.
Osmolality: Delivering parenteral nutrition centrally (into the vena cava) allows extremely high osmolality solutions to be used, as the fast blood flow (~2-5 litres/minute) instantly dilutes the solution. A peripherally delivered solution should have an osmolality <900 mOsm/kg to avoid irritation to the blood vessels. Lipid has a much lower osmolality than amino acids, glucose or electrolytes, so peripheral solutions are typically high in fat.
Hang-time: Interaction between the macronutrients and/or micronutrients can reduce the availability of the nutrients and decrease the stability of the solution. Shelf-life can be prolonged by keeping macronutrients separated (as in a multi-chamber bag) and/or by adding micronutrients into the solution as close as possible to the starting hang time of the infusion.
Bacterial growth: Lipid solutions have a lower osmolality and acidity than amino acids or glucose solutions, and therefore provide a better growth medium for bacteria. The hangtime for lipid on its own is shorter than for three-in-one solutions at 12 hours. Most TPN solutions are hung for a maximum of 24 hours.
Stability: Loss of stability (i.e. where the lipid ceases to be fully emulsified or where compounds precipitate out of solution) can make the parenteral nutrition formula unsafe for infusion. Several factors impact stability including: multi-chamber bags (longer shelf-life) vs. individually-compounded bags (shorter shelf-life), and storage practices (temperature, light, and shelf-life).
Additives: Each solution has an upper limit for nutritional additives (i.e. electrolytes or micronutrients) and these additives should be discussed with the pharmacist to ensure safety and stability. Because PN solutions are complex, it is typically not recommended to mix any medications with PN or infuse them through the same lumen. A commonly made exception is insulin, which can be added to the PN solution. If insulin is added to the PN solution, frequent blood glucose monitoring is essential for the entire time that parenteral nutrition is infusing.